As in all medical specialties, timely documentation and transcription is crucial in dermatology. Based on the recommendations from the Electronic Medical Records (EMR) Mandate, all healthcare providers are required to convert all medical charts into digital format. Dermatologists treat many skin conditions ranging from acne to skin cancer. They may have to perform a broad range of procedures on many patients. Many practices rely on EHR-integrated dermatology transcription services to handle their EHR documentation tasks.
EHRs streamline communication, increase charting efficiency, improve documentation accuracy, simplify administrative and financial tasks, and enhance physician and staff productivity. Advanced dermatology-specific EHR software come with templates and features that simplify the care delivery, documentation, and billing processes.
Let’s take a look at 5 best EHR software for dermatologists –
Nextech

This dermatology EHR system is customizable for most practice’s workflows. Its medical and cosmetic templates are tailored to meet each provider’s unique charting preferences. It offers views of all relevant patient details, streamlining the encounter and documentation process. This software uses smart stamping and 3D anatomical models to pre-populate exams, assessments, treatment plans and billing codes, all with a single click. This HIPAA-compliant system can also improve productivity and time management with talk-to-text dictation and voice commands from within the EHR.
EMA Dermatology

This easy touch-based dermatology EMR solution can clearly understand practice patterns and eliminate the need for templates. Designed for use on the iPad, EMA software brings a new touch screen approach to cloud-based EMR systems. Based on the unique username, it can recognize each practice’s preferred methods and even suggest top diagnoses and treatments. It enables providers to run powerful analytics and studies for value-based medicine in the form of MACRA and MIPS regulations. Its key features such as Outcomes and Grand Rounds can help evaluate and create clinical data from the nationwide dermatology community and provide a quick snapshot of patient progress and common treatments for specific diagnoses. Being cloud-based, providers can use this EHR virtually wherever and whenever they want.
DrChrono
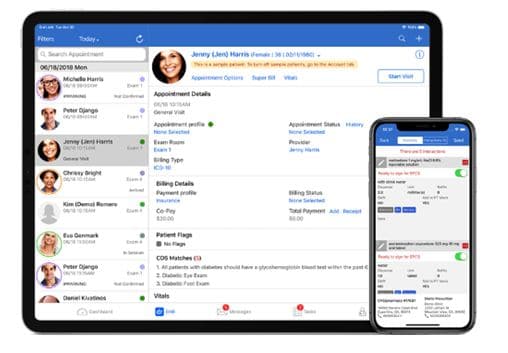
This advanced EHR system minimizes paperwork and errors by auto-populating patient information to clinical charts, procedures, and lab and radiology orders. The software comes with key features such as convenient e-prescribe medications, options to take HIPAA compliant photos of patient’s condition, and medical templates, making it an ideal platform for dermatologists. Its comprehensive dermatology medical forms are designed to meet the specific needs of the practice and its real time eligibility Insurance Check provide verification of payment.
Practice Fusion

This custom-tailored EHR for dermatologists is well known for its overall performance, scalability, reliability, training, meaningful use, and support. This software makes charting a more natural and intuitive process with less clicking and typing, offering providers more time to focus on patients. This platform can customize each provider’s EHR workflow to suit their needs while maintaining a single administrator. Its specialty-specific customizable flowsheets allows providers to quickly track patient health data, identify gaps in chronic care, and view historic lab results during the encounter.
Kareo Clinical
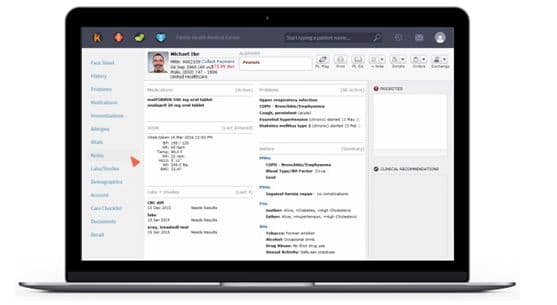
Designed and managed by healthcare providers, this cloud-based EHR makes it easy for dermatologists to write notes and prescriptions, code encounters, and manage patients. This fully integrated, cloud-based EHR features a comprehensive dashboard, simple charting options, easy e-prescribing, convenient eLabs, electronic superbills, and integrated patient portal.
How Dermatology Transcription Service Providers Can Help?
Documenting patient histories, surgical therapies, microbiology and biopsies in the EHR can be complex. Dermatology has specialized terms not seen in other medical fields. To improve EHR documentation, dermatologists can rely on EHR-integrated dermatology transcription services. A reliable medical transcription company can ensure that all clinical data is captured correctly in the EHR system in a timely manner, so that it is readily available for review by all healthcare providers and physicians involved in the patient’s care.
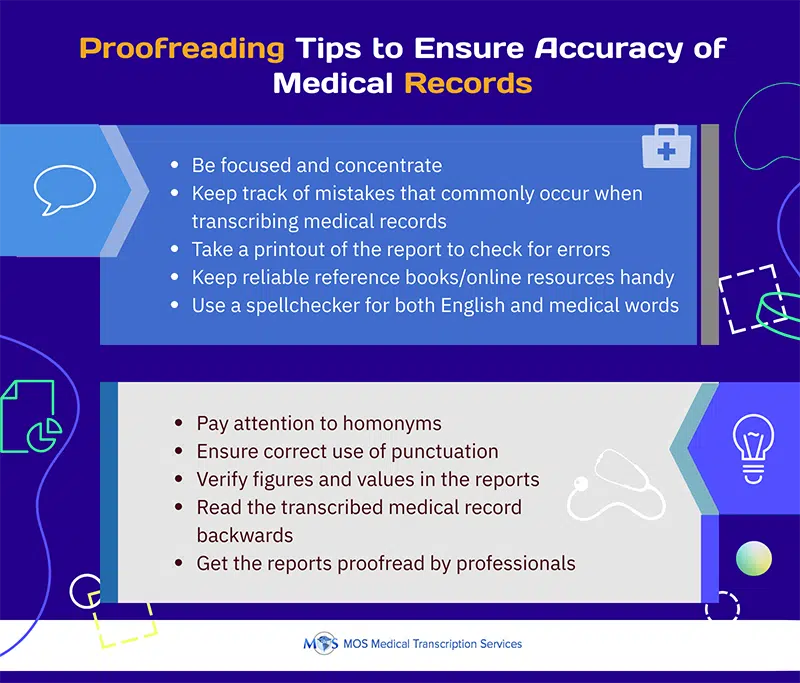
Accuracy in transcription is crucial to record pertinent facts, findings, and observations regarding a patient’s health history, past and present illnesses, examinations, tests, treatments, and delivery of care. Experienced transcriptionists are also familiar with the medical terminologies specific to all dermatology subsets such as cosmetic dermatology, dermatopathology, immunodermatology, Mohs surgery, pediatric dermatology and dermatoepidemiology, as well as all dermatologic therapies and medications. By helping physicians manage tedious and difficult EHR data entry tasks, medical transcription service providers can maximize dermatology practice efficiency, ensure access to accurate and timely documentation, and support delivery of quality care.
So regardless of the EHR system you choose, make sure that the medical transcription service company you partner with is HIPAA compliant and can ensure error-free and timely clinical documentation.