
Well-designed EHRs and EMRs are the backbone of the healthcare system. Though both the terms are used interchangeably and have some common features, they are different concepts. Both are essential to meet the nation’s goals of improving patient safety, and the quality and efficiency of patient care, and to reduce healthcare delivery costs. While EHR is an appropriate choice to share important information with other healthcare stakeholders, EMR would be the best option for a specialty practice to provide personalized healthcare for each patient’s needs. Physicians can rely on a reliable medical transcription service to ensure accurate and timely documentation in these systems. Understanding the transition from EMR to EHR is important for healthcare providers to determine which application to choose and how it will affect their organization.
Electronic Medical Record (EMR)
The Office of the National Coordinator for Health Information Technology (ONC) defines EMRs as digital versions of the paper charts in clinician offices, clinics, and hospitals. An EMR comprises a patient’s medical history that is maintained by a single provider. The EMR system contains the following health information:
- Demographic information
- Medications
- Allergies and immunizations
- Lab results, radiology reports and visits
The EMR may also include billing information and insurance information.
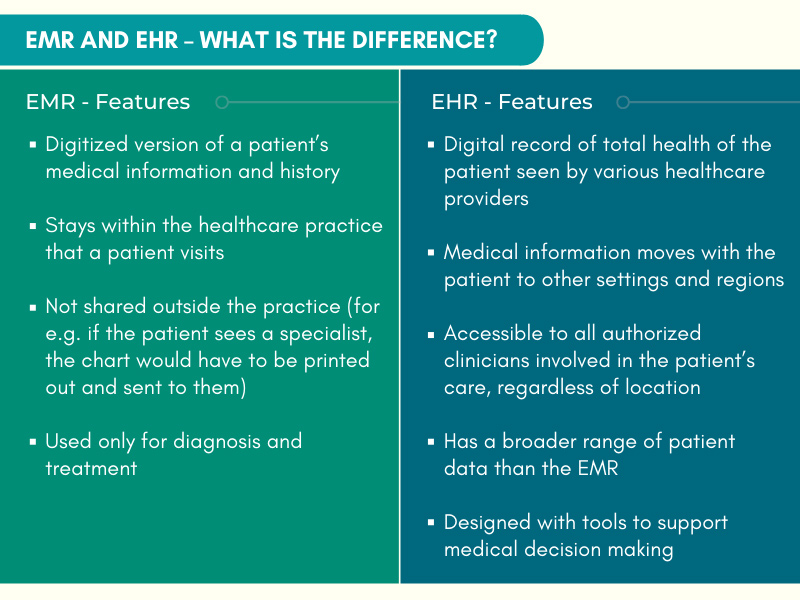
As the EMR contains the patient’s medical and treatment history collected within a single healthcare organization, the system remains in that organization and is used by its clinicians. EMRs are not shared outside the organization. Providers use the EMR for diagnosis and treatment. A medical transcription company that provides EMR-integrated transcription services can ensure complete, accurate and timely documentation of a patient’s medical history, tests, diagnosis and treatment in the system, which is crucial for appropriate care throughout the healthcare organization.
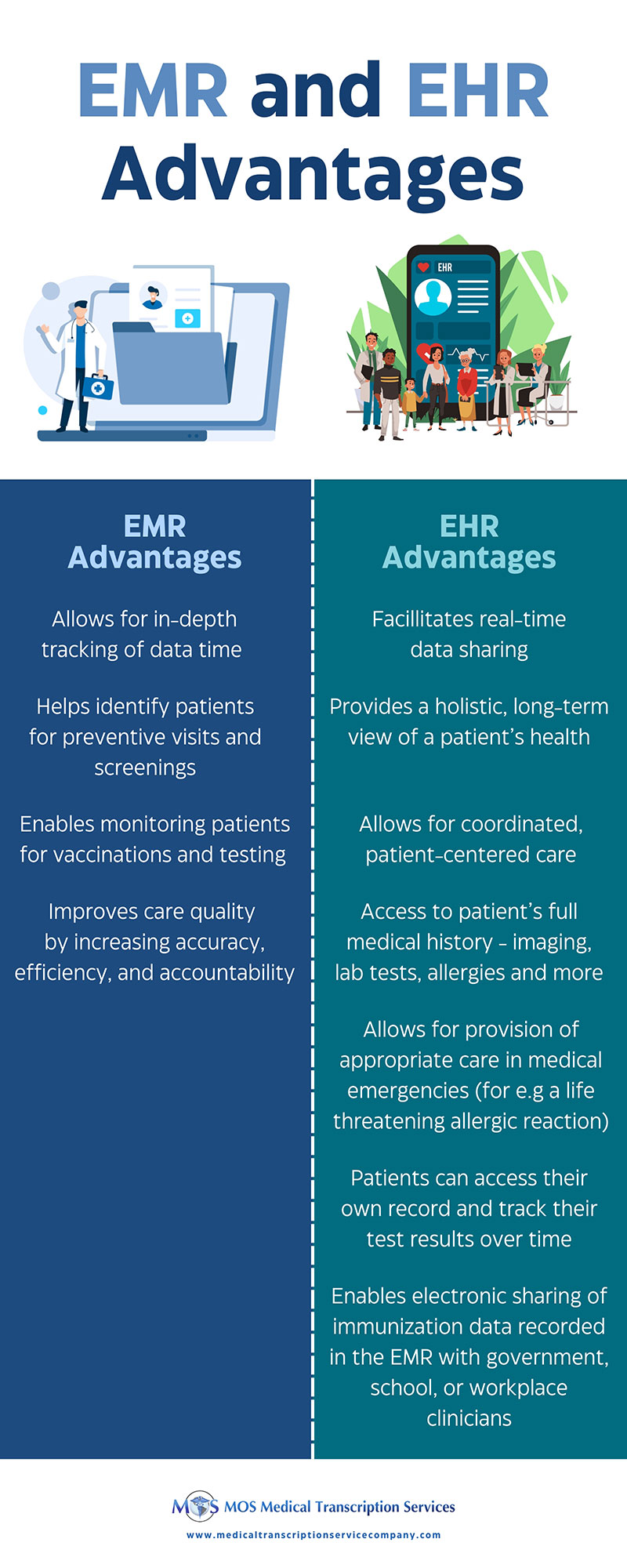
EMRs improve the quality of care in a healthcare practice/organization by helping their physicians monitor care by:
- Tracking data over time
- Identifying patients for preventive visits and screenings
- Monitoring patients for vaccinations and testing
- Improving care quality by increasing accuracy, efficiency, and accountability
If a patient switches physicians or seeks care from an outside specialist, the information in the patient’s EMR may have to be printed out and sent to them by mail. Specialty EMRs feature customized templates. For instance, in a cardiology practice, specialized cardiology EMR software along with cardiology transcription services can improve healthcare delivery.
Electronic Health Record (EHR)
Similar to the EMR, the EHR also contains demographic information, medications, allergies, immunizations, lab results, radiology reports and visits, and often, billing information and insurance information. However, the EHR system has both a broader and deeper scope than the EMR system. The ONC explains: “Electronic health records (EHRs) are built to go beyond standard clinical data collected in a provider’s office and are inclusive of a broader view of a patient’s care. EHRs contain information from all the clinicians involved in a patient’s care and all authorized clinicians involved in a patient’s care can access the information to provide care to that patient”.
What are the key features that distinguish EMR and EHR, including usability within a single provider versus data sharing across networks? While EHRs perform all the functions of EMRs, they are all-inclusive, much more complex, and reach out beyond the health organization that originally collects and compiles the information. The differences between EMR and EHR come down to accessibility and scope. EMRs are maintained by a single provider, while EHRs are maintained by multiple providers. EHR data can be created, managed, and accessed by authorized clinicians and staff across more than one healthcare organization as well as by patients themselves. As a result, EHRs contain more comprehensive information than EMRs. Providers primarily use EMRs for diagnosis and treatment purposes.
Furthermore, EHRs are designed to be interoperable, while EMRs are not. EMR and EHR interoperability refers to the ability of different systems to share and use data with each other. This is crucial because it enables providers to access a patient’s complete medical history, even if they see multiple providers. EHRs facilitate the transfer of a patient’s medical information to specialists, labs, imaging centers, emergency rooms, and pharmacies both locally and nationally.
EHRs:
- Focuses on the overall health of the patient by going beyond standard clinical data collected in the provider’s office
- Provides a broader view on a patient’s care
- Allows the patient’s medical record to follow them to other healthcare providers, specialists, practices, hospitals, nursing homes, including across states
- Allows clinicians access to a broader range of patient data than EMRs
A fully functional EHR can provide all members of the patient’s team with instant access to the latest information. The advantages of EHRs are:
- They enable better coordination of patient-centered care.
- In the event of a life-threatening condition, appropriate care can be provided even if the patient is unconscious.
- Patients can access their own medical records and review their test results from the previous year. This can promote medication adherence and assist them in maintaining lifestyle changes.
- Clinician notes from the patient’s hospitalization, discharge instructions, and guidance on follow-up care enable a seamless transition from one care setting to another.
- A fully integrated EHR system encompasses practice management, medical billing, and interfaces with pharmacies, laboratories, radiology departments, and other healthcare facilities.
EMR vs EHR is a discussion that also touches on practical outcomes: EHRs reduce time spent searching for records, cut redundant testing, and enable smarter care decisions. In contrast, EMRs enhance care within a single network, making them more useful in small or specialty practices. An expert medical transcription business offers affordable documentation solutions that are integrated with electronic health records.
EMRs enhance the quality of care that patients receive, especially when a patient visits different providers within the same network of clinics, by enabling providers to keep track of a patient’s medical history in one place. This is also beneficial for small practices with fewer patients.
To sum up, EHRs go a lot further than EMRs.
EHR and EMR – Many Benefits
Though they are different concepts, both EMRs and WHRs are essential to meet the nation’s goals of improving patient safety, and the quality and efficiency of patient care, and to reduce healthcare delivery costs, according to Dave Garets and Mike Davis, the authors of a 2006 HIMSS Analytics white paper (www.ehrintelligence.com).
They noted that EMR is the foundation on which EHR interoperability is built. “The EMR is the legal record created in hospitals and ambulatory environments that is the source of data for the EHR,” they wrote. “The EHR represents the ability to easily share medical information among stakeholders and to have a patient’s information follow him or her through the various modalities of care engaged by that individual. Stakeholders are composed of patients/consumers, healthcare providers, employers, and/or payers/insurers, including the government.”
Well-designed EHRs and EMRs are the backbone of the healthcare system. In a general practice, where providers need to share information with other healthcare stakeholders, an EHR would be the appropriate choice. On the other hand, an EMR would be the best option for a specialty practice to provide personalized healthcare for each patient’s needs. Partnering with a professional medical transcription service organization in the USA can ensure error-free documentation in EHR and EMR systems.


