As a provider of medical transcription services, we assist small and large clinics, multi-specialty clinics and group practices, and individual physicians practicing in any specialty in improving their office efficiency. Our medical transcription service is designed to improve the way you work. We serve all major specialties. Our blogs are focused on highlighting the importance of medical transcription, the latest news, updates, and events in the transcription industry.
As we are heading to a New Year, here’s a look back at some of our most insightful blog posts of 2020. This is an opportunity to learn from the best in business. Read on!
- Impact of Medical Terminology on Patient Care
Proper physician-patient communication is an essential element of care. Medical terminology is the standardized language that allows healthcare providers, HIM professionals and medical transcription service companies to communicate on a patient’s condition and medical needs. This blog highlights the impact of medical terminology on patient care.
- Study Analyzes CBT Transcripts using AI to Identify Benefits of Psychotherapy
Providing access to mental health treatment in a timely manner is critical to improving patient well-being. Psychiatrists and psychologists who use telehealth can see patients in their own homes via digital platforms and high-speed Internet service. Read about a study thatd extracted data from cognitive behavioral therapy session transcripts using advanced algorithms to drive care improvements.
- Using Telemedicine for Patient Care during the COVID-19 Pandemic
Telemedicine and telehealth have been around in the U.S. since the 1950s. The COVID-19 pandemic has put the spotlight on telemedicine as an effective way to connect patients, physicians and health systems. With telemedicine, vulnerable patients can receive virtual care without having to visit a healthcare center or physician office. This blog discusses how virtual healthcare was used during the coronavirus crisis.
- Key Tips to Keep Your Medical Practice Running during COVID-19
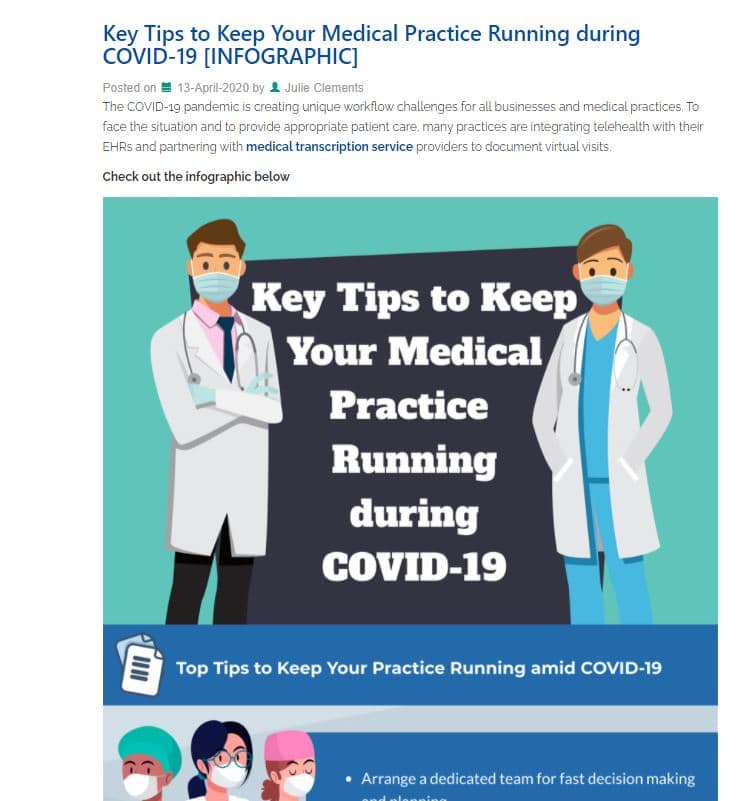
Medical practices across the country are facing unique business and workflow challenges due to COVID-19. To keep their medical practices running, physicians need to adapt to the new requirements demanded by COVID-19. This infographic provides tips on how to run a medical practice efficiently.
- Are EHRs Equipped to Deal with COVID-19?
EHRs are a reliable source of data for disease symptoms, laboratory results, and treatments. With the emergence of the novel coronavirus disease, it is imperative that EHR data use in public health surveillance activities continues to increase. Researchers say that COVID-19 will be “the ultimate stress test” for EHRs, with challenges such as evolving workflows, data demands and cyber threats. Check out this blog, for more detailed information.
- Ensuring HIPAA Compliance with Widespread Remote Work Adoption
In recent days, many organizations have switched to remote work due to the pandemic. Healthcare providers should take extra precautions to ensure the confidentiality of patient data when staff switch to working from home. This blog includes 8 steps that healthcare organizations can take to set up remote workspaces for HIPAA adherence.
- Implementing Telemedicine during this COVID-19 Crisis and Preparing for a Changed World
Telemedicine has been around for a long time, however, adoption of technology for virtual patient consultations progressed at a slow pace due to barriers such as cost, state licensure, and lack of good reimbursement. All of that has changed in recent times, especially with the coronavirus pandemic. Telemedicine can help physicians deliver care safely to non-urgent patients during the COVID-19 pandemic and will likely become the norm. This blog has rounded up guidelines from the American Medical Association (AMA) and industry experts to expedite implementation of telemedicine.
- Best Practices for Conducting Telemedicine Visits
The COVID-19 outbreak has put the spotlight on telemedicine. It is proving to be an effective option to meet the care challenges created by the pandemic. As the use of telemedicine becomes widespread, healthcare providers and patients need to understand how the technology works to ensure a positive patient experience. The blog discusses some best practices for conducting telemedicine visits.
- How Healthcare Organizations Can Better Manage EHR Data Growth

Electronic heath records (EHRs) are a treasure trove of patient information. If managed efficiently, EHR data can provide meaningful insights and help physicians make informed decisions to streamline operations, enhance patient care, and attain better outcomes. See how healthcare organizations can better manage EHR data growth.
- Seven Things that Today’s Patients Expect from Medical Practices

All physicians are focused on providing the best care and ensuring that each patient experience is a positive one. In fact, taking steps to improve the patient experience can attract new patients and increase patient retention. While it is the quality of care that really matters, there are certain other things also that patients expect from medical practices. Check out this blog for more information.
Thank you so much for supporting our business in 2020. We’re looking forward to serving you again in 2021!
Wish you all a spectacular New Year!

![6 Common Causes Of Medical Errors [INFOGRAPHIC] Medical Errors](https://www.medicaltranscriptionservicecompany.com/wp-content/uploads/2020/12/6-common-causes-of-medical-errors.jpg)