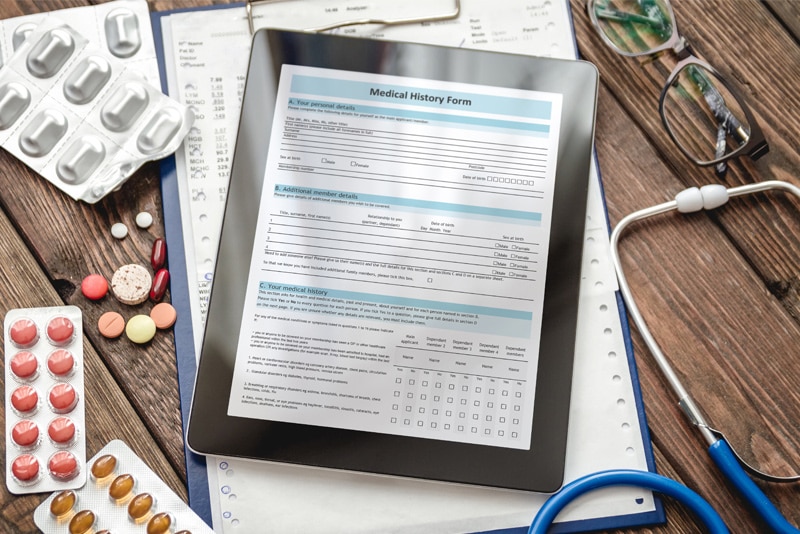
Patients’ adverse reactions to medications and allergies to food and other substances are an important component of documentation that medical transcription service companies specializing in allergy and sleep medicine transcription can help physicians like yourself with. It is important to document a complete and accurate allergy history for each patient. Accurate and timely documentation of allergies in electronic health records (EHRs) is critical for you to be better prepared for adverse events and ensure proper care.

The Joint Commission and the Accreditation Association for Ambulatory Health Care (AAAHC) require providers to document drug allergies and their reactions in a “highly visible location in the patient’s chart”. The Centers for Medicare and Medicaid (CMS) also require documentation of patient drug allergies and associated reactions in the Conditions for Coverage section.

The Agency for Healthcare Research and Quality’s (AHRQ) has stated that all health care professionals involved in a patient’s care should have the ability to record both drug allergies and adverse drug reactions. Only clinicians with direct knowledge of the patient should be permitted to change these labels and discuss any potential change in assignment (allergy vs adverse drug reaction) directly with the patient before the change is made.

Best Practices for Documenting Allergies in Patient Records – what Physicians and Allergy and Sleep Medicine Transcription Providers Should Know:
- Create an Accurate Record of the Patient’s Allergy History: You should discuss allergies with your patients at each visit and correctly record existing or new allergies and reactions. A Relias media article references Belle Lerner MA, director of research at the AAAHC Institute for Quality Improvement as saying that these discussions are also important to understand if the patient has an allergy or a COVID-19 symptom. The key is to get as much information as possible from the patient.
- Educate Staff: Practice staff must be educated about all types of allergies, including food, latex, mold, and drugs as well as symptoms and what to look for. Typical drug allergy reactions include: skin rash or hives, itching, wheezing or other breathing problems, swelling, and anaphylaxis, a reaction that can affect two or more organ systems and be potentially life-threatening. Staff should also be trained to handle adverse events properly.
- Ensure Consistent and Up-to-Date Patient Documentation: Lerner points out that documenting the type and severity of reaction is essential for crucial allergy decision-making. Make sure the documentation includes all prescription medications and supplements as well as over-the-counter vitamins, medications, and supplements. Drug allergy status should be documented in all communication regarding the patient between health care providers.
- Medication Reconciliation: Comparing a patient’s medication orders to all of the medications that the patient has been taking or medication reconciliation can avoid errors such as medication omissions, duplications, dosing errors, or drug interactions. Best practice is to do this at every care transition during which new medications are prescribed or existing orders are rewritten.
- Standardize Procedures: Documentation of a drug allergy in the patient record should include the reaction, the drug administered, the timeframe of the reaction from when the drug was given, and the drugs to avoid. EHRs can include prompts alerting patients to provide updated allergy information to their pharmacy, which can minimize confusion. If medications are ordered in the surgery center, surgery staff should share all allergy documentation and information with the primary care provider and the pharmacy. This crucial for smooth transition of care.
Despite the importance of good allergy documentation, the Agency for Healthcare Research and Quality (AHRQ) reported that the majority of EHR allergy modules have serious drawbacks when it comes to documentation allergies and triggering drug allergy alerts.
Limitations of the majority of EHR allergy modules include:
- Frequently missing documentation of reaction mechanism and type
- Absence of a comprehensive terminology
- Lack of adequate tools for reconciling allergy information, and
- An allergy alert override rate of greater than 90 percent caused by physician alert fatigue
The AHRQ project to improve allergy documentation and clinical decision support in the EHR aims to provide clinicians at the intervention sites with access to an allergy reconciliation module in the EHR.
Correct and complete documentation is crucial to deliver patient care in a safe environment. As you focus on treating allergies, you can rely on a medical transcription company that provides allergy and sleep medicine transcription service to ensure timely and accurate documentation of allergies in the EHR.