Emergency departments (EDs) are at the frontline of care during the coronavirus pandemic and medical transcription companies are focused on meeting need for prompt and accurate electronic health record (EHR) documentation. One significant development since the pandemic began is the increased use of telemedicine in emergency care. This trend was supported by the easing of regulatory and administrative barriers in telemedicine. By limiting face-to-face interactions, tele-triage keeps both patients and clinicians safe, and prevents the spread of the virus.
Benefits of Telemedicine for Emergency Care during the Pandemic
With telemedicine services, healthcare providers and their patients can stay connected and communicating from anywhere. When the pandemic broke out, virtual platforms allowed emergency physicians to triage patients outside the four walls of the hospital. Telemedicine was used to help providers determine whether patients needed to visit the ED or if a virtual consultation would be sufficient. By directing patients to the appropriate setting, physicians could emergency department overcrowding at a time when resources had to be safeguarded for treatment of severely ill COVID-positive patients. Tele-triage also became an important method to identifying patients who were possibly infected with COVID-19, but who did not need emergency care and could remain under home isolation, reducing the risk of transmission to front-line health care workers and other ED patients.
A paper published on Wiley Online Library in May 2021, discusses studies that evaluated the pandemic‐related uses of telehealth in emergency care in five areas:
- Pre‐ED/Prehospital: Telehealth has functioned as a screening tool for patients with emergency care needs and to support care coordination in the pre‐ED setting. By facilitating per-hospital evaluation, telehealth services weeded out non-emergency situations from those needing serious attention. Patients with COVID 2019 exposure but no serious safety concerns could be directed to alternative testing locations instead of the ED.
- Within ED: EDs used telehealth as a tool to screen patients for acute care needs. This helped limit staff and patient exposure and conserved the use of personal protective equipment (PPE). Teleconsultations also allowed ED physicians to interact with specialist services and specialists to interact with patients. One study discussed how telehealth was used by an institution to coordinate transfers of emergency patients, enable remote ultrasound, and provide virtual consultations.
- Post‐ED discharge: Emergency departments have utilized telehealth following patients’ discharge from ED to extend care, especially for follow‐up and remote monitoring. EDs and skilled nursing facilities were used to triage patients discharged patients appropriately.
- Education: Telehealth platforms and digital tools have supported new educational initiatives and strategies, minimizing the need for in-person contact. Robust digital initiatives have made possible continued education for trainees, nurses, and physicians. Organizations are using iPads and telehealth to help with interhospital care coordination as well as telehealth to enable patients to self‐monitor vital signs.
- Care and Resource Coordination: Telehealth helped EDs and hospital systems coordinate and conserve scarce medical resources during the pandemic.
Even before the pandemic, telehealth supported EDs in many ways. Virtual care is a solution for overcrowding in emergency departments and urgent care centers. It is a useful option for older adults with chronic conditions on a lot of medications, when transition of care becomes critically important. Video-based consultations have helped physicians assess fevers in children, rashes in adults, abdominal pain and facial swelling. Patients could transmit information about their health and readings with at-home monitoring tools, enabling physicians to identify new symptoms, worsening health, and potential emergencies. This helped patients get life-saving interventions without delay. Telehealth is also a great option for mental health emergencies, allowing people to connect with a therapist at any time.
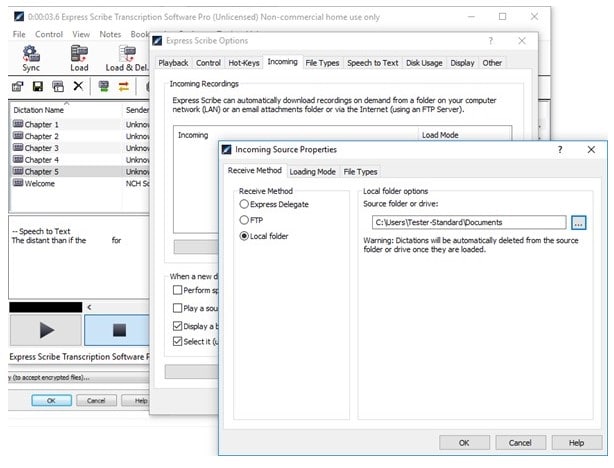
Telehealth Visits – Optimizing Documentation
Optimizing EHR documentation is essential so that ER physicians can focus their time and attention on patient care. If clinicians record patient information as notes in the EHR in real-time during a patient encounter, patient data can be shared among health providers. However, this practice is the main cause of clinician burnout. Telehealth undoubtedly has immense value in emergency care. Integrating a telehealth platform into the EHR and patient portal supported by EHR-integrated medical transcription services can reduce clinician burden and ease documentation. Even if clinicians use voice recognition technology to save time with EHR documentation, outsourcing medical transcription will ensure that physician dictation is edited and proofread to produce quality medical records.