Table of Contents
Accurate medical transcription is crucial for medical practices in all specialties to create the medical history of patients, to provide quality care, take better treatment decisions, for proper documentation and to get reimbursements on time. Medical transcriptionists performing the task must be well-versed in the process they’re dealing with, as even a single error in the reports could impact the treatment decisions. Professional medical transcription services provide training for their staff to keep them up to date and current.
Importance of Medical Transcription Reference Books and Tools
To achieve high-quality healthcare documentation, professional transcriptionists use the various medical transcription tools and resources. These include reference materials such as medical dictionaries, drug reference books, and specialty word books. These resources help them accurately decipher complex terminologies and produce precise transcripts. Both novice and experienced transcriptionists can benefit from these references to enhance their skills and knowledge.
Medical reference materials such as dictionaries, medical books, drug reference books, medical specialty word books and English language dictionaries can help transcribers figure out the exact terminologies and words in the recording and generate accurate transcripts. Both fresh and experienced medical transcriptionists can use these references to build their career. Online resources such as OneLook, Transcription Gear, Drugs.com, and Healthy Computing can help them get familiar with medical words, phrases, acronyms or abbreviations related to medical transcription in different specialties. Experienced medical transcription service companies have professionals skilled in transcribing all types of medical reports including medical history, physical examination reports, operative reports, discharge summaries, emergency room reports, chart notes, medical evaluations, and more.
Sometimes medical transcriptionists receive audio files that are of poor quality and have background noise or speakers who talk too fast, making it difficult to decode the provider’s intended choice of words. Having medical reference materials can help them figure out the exact terminologies and words mentioned in the recording and produce accurate transcripts.
Must-have Resources for Professional Medical Transcriptionists
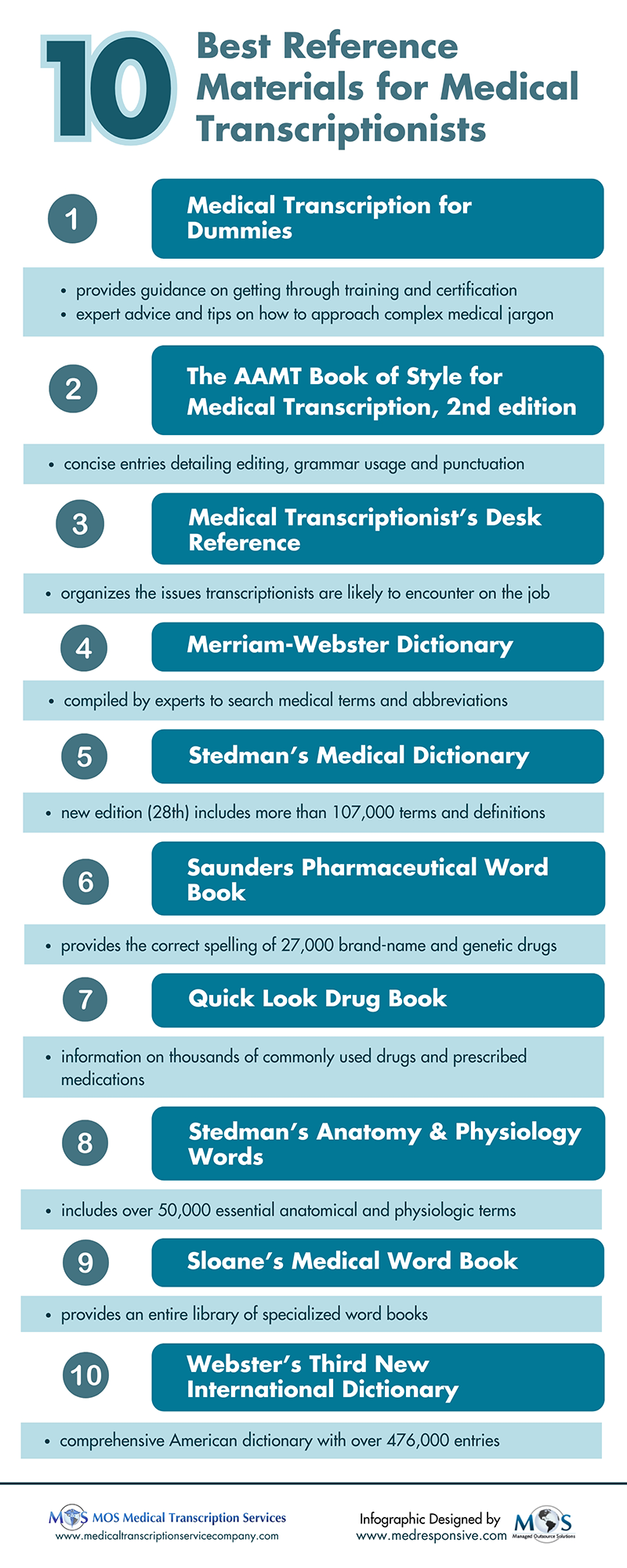
Let us check out the reference materials available for medical transcriptionists.
Reference books for accurate transcription: Diverse medical transcription books are available for fresh and experienced transcriptionists to build their career in the world of medical transcription.
- Medical Transcription for Dummies: Medical Transcription for Dummies provides guidance on getting through training and certification, and exploring opportunities. This book also includes expert advice and tips on how to approach complex medical jargon and understand procedures, and plain English explanations of medical terminology, anatomy and physiology, diagnostic procedures, pharmacology, and treatment assessments. Students as well as professional medical transcriptionists alike can benefit from Medical Transcription for Dummies.
- The AAMT Book of Style for Medical Transcription, 2nd edition: When transcribing notes for medical providers, it is important for the transcriber to know and use the rules of medical transcription. The AAMT Book of Style for Medical Transcription is really helpful, as it comes with concise entries detailing points about editing, grammar usage, punctuation and much more. Referred to as “the gold standard” for medical transcriptionists, this book has a comprehensive index completed by a professional indexer.
- The 2nd edition of the Book of Style reflects many improvements suggested by users of the book over the years. It includes a comprehensive index prepared by a professional indexer. The new book also reflects some changes in documentation practices.
- Medical Transcriptionist’s Desk Reference: Written by an experienced medical transcriptionist, this reference book properly organizes the type of problem or issue transcriptionists are likely to encounter on the job. Transcribers can easily find solutions to the most common problems they face, making the task of transcribing medical reports easier and more efficient. Following the AAMT style guidelines, this book also provides quick access to facts related to anatomy, general medical terminology, and various medical specialties.
Medical dictionary
A standard medical dictionary can help seek out and reference any complex medical terms that are spoken in the audio files recorded by physicians.
- Merriam-Webster: Transcribers can use this dictionary compiled by experts to search medical terms and abbreviations. The new edition of this dictionary provides a concise guide to the essential language of medicine with more than 38,000 entries and over 500 new words and senses. Pronunciations are also provided for all entries and it covers the latest brand names and generic equivalents of common drugs. Some new words included are – diabesity, gastric banding, and micro fracture.
- Stedman’s Medical Dictionary: It is the most reliable resource available for healthcare specialists of all kinds – medical students, physicians, transcriptionists, educators, researchers, and medical language specialists. The new edition (28th) of Stedman’s Medical Dictionary includes more than 107,000 terms and definitions. All the terms are explained clearly with approximately 1,500 images and illustrations. Transcribers can also make use of the CD-ROM that has audio pronunciations, anatomical animations, and a spell checker.
Drug reference book
Doctors often dictate the drugs they have recommended to the patient. Without clear knowledge of those drugs, the transcriptionist may be confused, whether the name of the drug or brand name is being dictated.
- Saunders Pharmaceutical Word Book: Medical transcriptionists can work more quickly and accurately with the information organized in this book. It provides the correct spelling and capitalization of over 27,000 brand-name and generic drugs with dosage forms, investigational drug names and codes, chemotherapy protocols, trademarked dosage forms, and drug categories/classes. It also contains the indications of approved drugs and standard dosages.
- Quick Look Drug Book: Medical transcriptionists can use this resource for information on brand and generic drug names, pronunciations, look-alike/sound-alike issues, therapeutic categories, dosages, and dosage forms. The 2009 version of this book includes the most current information on thousands of commonly used drugs, along with a 32-page color insert showing the 200 most commonly prescribed medications. The recent version includes new drugs introduced or approved by the FDA in 2008.
Medical specialty word book
For transcribing an audio file that deals with a medical specialty like radiology, orthopedics or any other, transcribers need to be familiar with terms related to this specialty.
- Stedman’s Anatomy & Physiology Words: In the second edition of Stedman’s Anatomy & Physiology Words, there are over 50,000 essential anatomical and physiologic terms. Its appendix includes anatomical illustrations, a list of English-Latin anatomy words, and tables of ligaments and tendons, muscles, bones, arteries, and nerves.
- Sloane’s Medical Word Book: Students and practicing transcriptionists can make use of this single reference to get an entire library of specialized word books. Terms are clearly organized by specialty, making it easy to select the correct word with accuracy. It explains general medical terms, general surgical terms, and laboratory, pathology, and chemistry terms and specialties includes terms from 18 different specialties.
English language dictionary
Transcribers can use an English language dictionary to look up the correct spelling and meaning of certain English words spoken in the medical audio files.
- Webster’s Third New International Dictionary: This is the largest and most comprehensive American dictionary available with over 476,000 entries. It also features a special updated Addenda Section of new words and meanings. It comes with 3,000 illustrations and 140,000 etymologies describing word origins as well as 200,000 verbal illustrations and quotations.
By improving transcription accuracy with reference materials, medical documentation specialists ensure accurate and reliable clinical documentation supporting patient care and legal purposes. Reliable medical transcription service companies employ scribes who are experienced in transcribing all types of medical reports including medical history, physical examination reports, operative reports, discharge summaries, emergency room reports, chart notes, medical evaluations, and more. Additionally, partnering with HIPAA compliant transcription services ensures that sensitive patient data is handled securely and in compliance with regulations.