Table of Contents
A chiropractor can have a large number of health records to deal with on a weekly basis, and that means a lot of notes that must be transcribed. This process can take a great deal of time, which could mean less time spent seeing patients or a backlog of paperwork. This problem can be resolved by working with a reputable medical transcription service that can generate accurate chiropractic medical records.
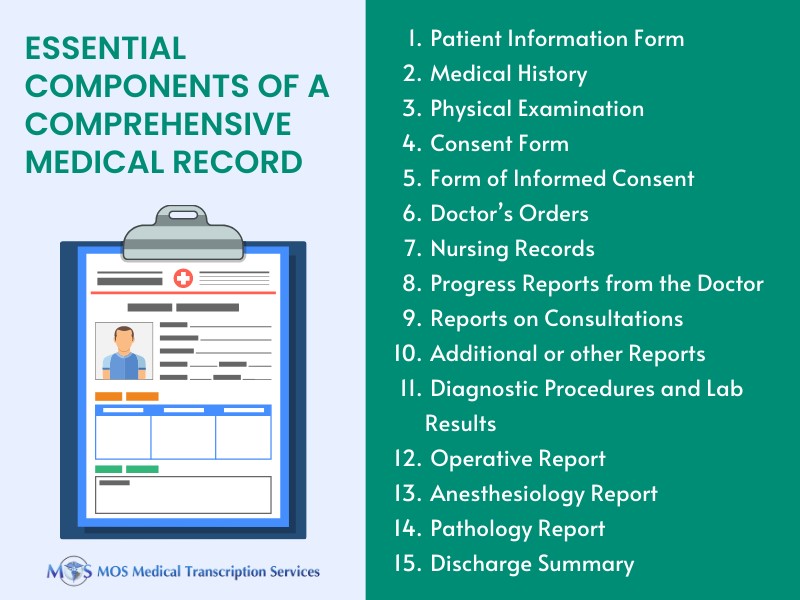
It is crucial to properly document each visit since it facilitates communication among healthcare professionals. It examines the care the patient received from the time of admission until discharge, covering issues like diagnoses, treatments, and the resources employed. Medical practitioners’ ability to communicate with one another is facilitated by accurate, detailed, and extensive documentation. Chiropractic doctors, like all other healthcare providers, are required to keep thorough records of all their patient interactions. This can safeguard both their patients and themselves.
Tips to Generate Accurate Chiropractic Records:
The following apply whether an x-ray or physical examination reveal the subluxation.
- The patient’s history that contains:
- The symptoms that led to seeking medical attention and also their primary complaint that brought them to the treatment.
- Details regarding the patient’s and his/her family’s overall health, any previous illnesses or injuries that could affect their treatment, any drugs they are now taking, and whether they have ever received chiropractic care.
- Details about current illness:
- the mechanism of trauma
- the quality and nature of the symptoms/problem
- Onset, duration, intensity, frequency, location, and the radiation of symptoms are all included
- Aggravating or relieving factors
- Prior interventions, treatments, medications, secondary complaint
- The degree of subluxation must be directly correlated with these symptoms. The symptoms should be stated as pain (algia), inflammation (itis), or as signals like swelling, spasticity, etc. They should pertain to the spine (spondyle or vertebral), muscle (myo), bone [sic] (osseo or osteo), rib (costo or costal), or joint (arthro).
It is insufficient to just declare that there is “pain.” It is necessary to define the pain’s location and verify whether the listed vertebra in question is able to cause it there.
- Assessment of the musculoskeletal and nervous systems via physical examination or x-rays:
Identify how it was established that the patient’s pain when they first arrived was caused by a subluxation. Two of the four P.A.R.T. criteria-one of which must be asymmetry/ misalignment or range-of-motion abnormality-must be met in order to identify a subluxation based only on a physical examination.
- evaluation of the location, nature, and degree of pain or soreness
- a sectional or segmental level asymmetry or misalignment
- abnormalities in range of motion
- alterations in the properties of adjacent or connected soft tissues.
- Diagnosis:
- The primary diagnosis must be subluxation, including level of subluxation, either as expressed or indicated by a phrase that describes subluxation. Such words may refer to the state of the affected spinal joint or the direction that a certain bone is moving in.
- To support the condition that led to the first diagnosis, secondary diagnostic is necessary.
- Each level of the spine that is modified and invoiced for requires notes to validate these diagnosis codes.
- Treatment plan:The following elements must be included in the treatment plan:
- The recommended level of care (length and frequency of visits)
- Specific treatment objectives
- Evaluation of treatment effectiveness using objective metrics
Some Documentation Tips
- Give thorough and readable documentation
- Clearly state the need for medical care
- Use standardized acronyms
- Include a treatment plan
- Provide specific date of service elements
- Specify which services are required
- Each level billed must be supported with documentation
- Be cautious when using software-generated documentation, as some may have similar items for several patients or service dates
- Be cautious when using check-off forms because they might be challenging to read, lacking in findings, overly general, and lacking adequate space to list all the necessary information
- Be cautious when including non-encounter specific repetitive items that lack the components required by policy and were rejected after evaluation
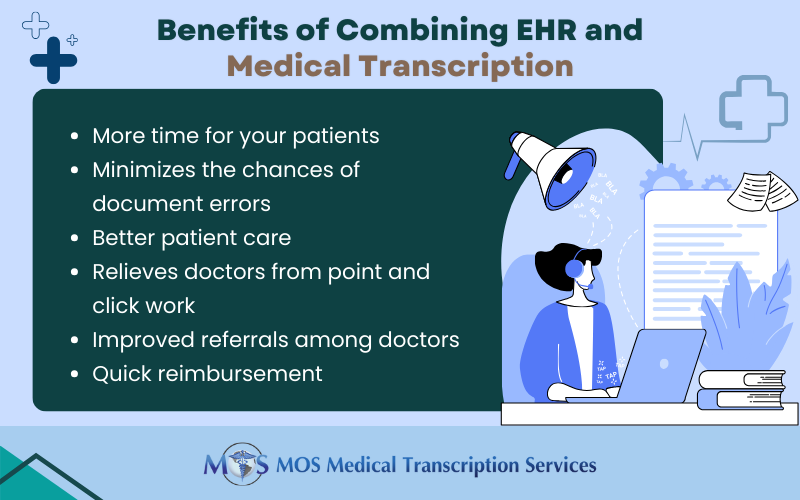
Like any other doctor, chiropractors are subject to audits and malpractice lawsuits. It’s crucial that you have quick access to accurate medical records in case either of these scenarios occurs. It also helps avoid the risk of being out of HIPAA compliance if you attempt to type out your own reports or have a member of your team transcribe them. To create reliable medical records for chiropractors, it is therefore best to get in touch with chiropractic transcription services or medical transcription services. It’s critical to have your claims and documentation reviewed to make sure they withstand scrutiny with an audit or investigation, and are in good health for the business as well as for improved patient care.