Maintaining proper mental health progress records is important for practices to provide patients with the care they need. EHR integrated mental health transcription services offer many benefits such as better collaboration among providers, improved medication management and crisis management, health information privacy and security, and much more.
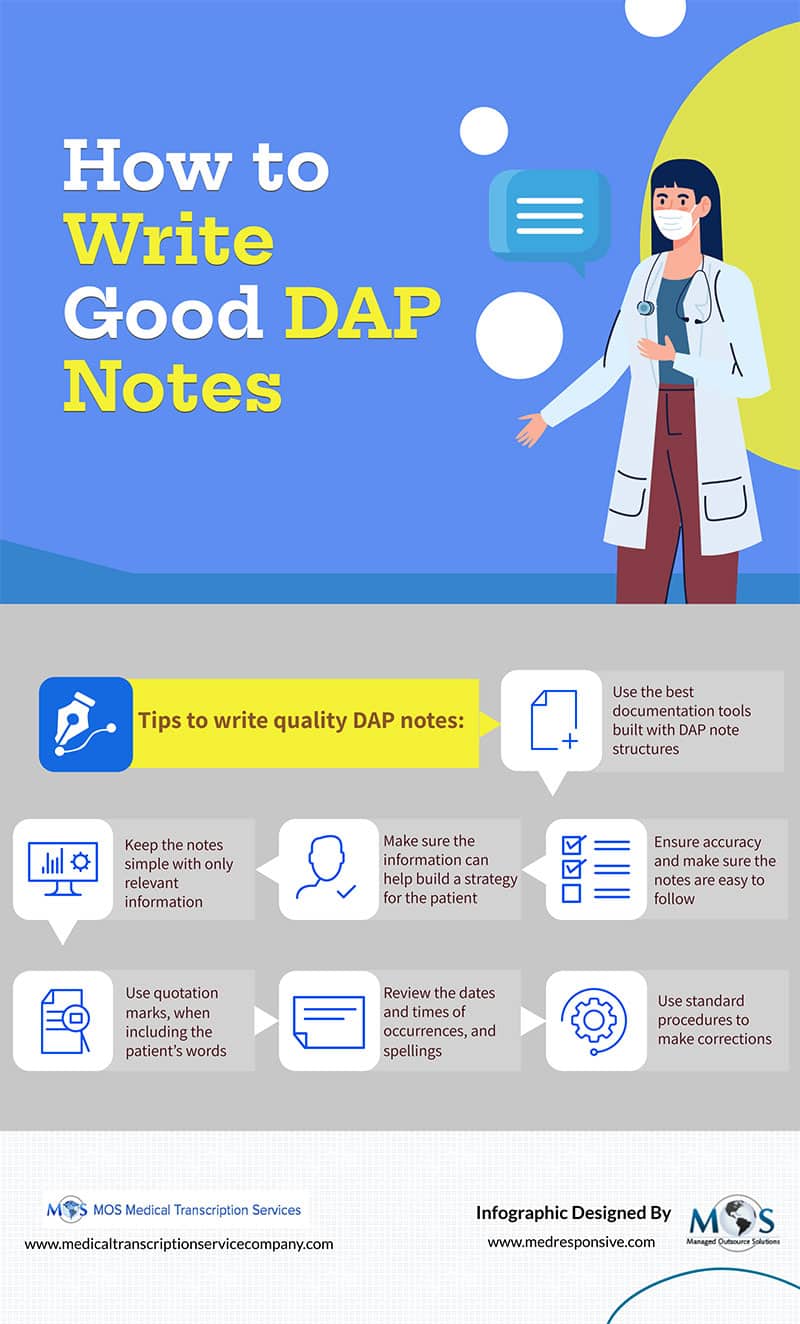
The two common mental health documentation methods are SOAP (Subjective, Operative, Assessment and Plan) and DAP (Data, Assessment, and Plan). While the main purpose of SOAP notes is to help providers monitor patients with multiple conditions, the DAP note aims to helping mental health professionals document and track the patient’s progress in an organized and efficient manner. DAP note merges the Subjective and Objective elements under the Data section.
Check out the infographic below
Read our blog on DAP vs SOAP Therapy Notes? What Are The Differences?
![Radiology Transcription Challenges Practices Face [INFOGRAPHIC]](https://www.medicaltranscriptionservicecompany.com/wp-content/uploads/2024/05/radiology-transcription-challenges-practices-face.webp)
![Medical Record Documentation Requirements For Podiatry [INFOGRAPHIC]](https://www.medicaltranscriptionservicecompany.com/wp-content/uploads/2023/05/medical-record-documentation-requirements-for-podiatry.jpg)