The flu season in the US usually runs from October to May and peaks in February. As healthcare providers grapple with feverish patients and take extra precautions to prevent the spread of flu, medical transcription outsourcing helps them maintain complete and legible documentation on immunizations, relevant details of patient consultations, and care provided. Complete and consistent medical record documentation is an important for influenza tracking to understand the severity of the outbreak and plan public interventions. New research has found that data provided by Fitbit devices could help inform timely and accurate models of population-level influenza trends. The Scripps Research Translational Institute study was published online in The Lancet Digital Health earlier this month.
The current flu outbreak is on track to be one of the worst in years, according to the Director of the National Institute of Allergies and Infectious Diseases (www.cnn.com). According to the CDC, this year’s flu season has led to at least 5.9 million medical visits and 120,000 hospitalizations, with 39 pediatric deaths reported as of Jan. 11. The Influenza Division at CDC collects, compiles and analyzes information on influenza activity year-round through a surveillance network that includes doctors’ offices and clinics. The key flu indicators that the agency uses include the percentage of influenza-like illness (ILI) visits to outpatient clinics, the rates of influenza-associated hospitalizations, and the percentage of deaths resulting from pneumonia or flu. Timely and accurate estimates of population flu tracking are necessary to:
- Understand the seasonality of influenza
- Determine the extent of the illness
- Identify and monitor groups at high risk of severe disease and mortality
- Recognize circulating viruses
- Indicate the start and end of the influenza season
- Help plan public interventions
However, according to the Scripps Research team, the CDC’s influenza-like illness (ILI) data are typically reported one to three weeks late and reported statistics are often revised months later. They noted that though Google Flu Trends and social media tools have attempted to capture real-time flu surveillance data, they have not been always successful.
The new study suggests that heart rate and sleep data from Fitbits devices can predict and alert public health officials to real-time outbreaks of flu more accurately than current surveillance methods.
“The ability to harness wearable device data at a large scale might help to improve objective, real-time estimates of ILI rates at a more local level, giving public health responders the ability to act quickly and precisely on suspected outbreaks,” the researchers wrote.
One of the most well-known names in fitness trackers, Fitbit wearable devices allow users to keep track of their activity. Fitbit devices measure daily steps, calories burned and distance traveled as well as floors climbed, sleep duration and quality, and heart rate. Newer Fitbit devices feature special hardware that provides blood oxygen data to help track health issues like asthma, heart disease and sleep apnea.
Researchers tested if Fitbit data could be used to improve prediction of flu outbreaks at the state level. This was based on the hypothesis that when sick, people’s resting heart rate, sleep patterns and daily activities change, and fitness bands or smart watches could help identify such fluctuations.
They tracked more than 200,000 US Fitbit users who wore their device for at least 60 days during the period March 2016 to March 2018. The average age of the Fitbit users was 43 and 60% were women. To measure population-level changes, data was collected from the five states with the highest Fitbit use: California, Texas, New York, Illinois, and Pennsylvania.
The researchers concluded that using RHR (resting heart rate) and other metrics from wearables has the potential to improve realtime ILI surveillance. They noted that Fitbit data improved flu predictions by 6% to 33% over baseline models.
“New wearables that include continuous sensors for temperature, blood pressure, pulse oximetry, ECG, or even cough recognition, are likely to further improve our ability to identify population and even individual-level influenza activity. In the future, with access to real-time data from these devices, it might be possible to identify ILI rates on a daily, instead of weekly, basis, providing even more timely surveillance. As these devices become more ubiquitous, this sensor-based surveillance technique could even be applied at a more global level where surveillance sites and laboratories are not always available,” they wrote.
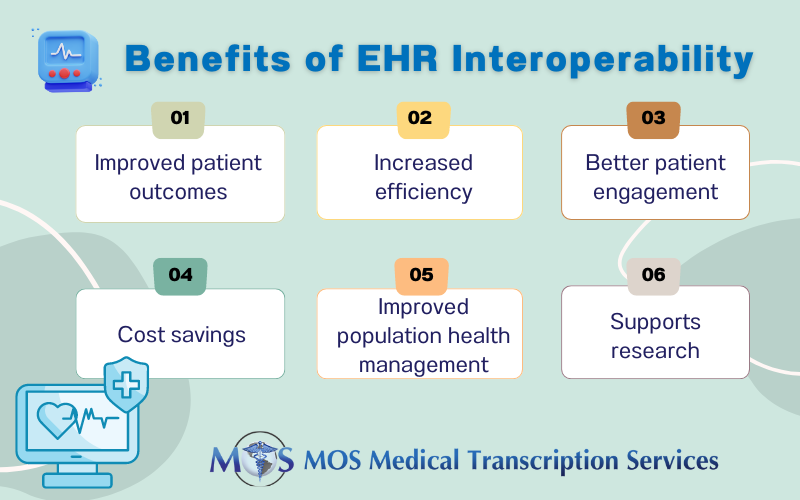
Real-time data from EHRs plays an important role in helping local public health authorities monitor and provide guidance for influenza and other outbreaks. In 2019, Healio reported on a study which found that real time data mining of EHRs can rapidly identify the transmission route or routes that are responsible for a hospital disease outbreak. Accurate and timely infectious disease transcription services can ensure comprehensive EHR data to help public authorities with infectious disease surveillance. Determining the influenza burden can help decision-makers prioritize resources and plan appropriate public health interventions.