A medical report provides a detailed account of a patient’s medical history, current condition, and treatment plan. Medical reports can be written by a variety of healthcare professionals, including doctors, nurses, and therapists, involved in a patient’s care. These reports help them track the patient’s progress, make informed decisions about treatment, and communicate with each other Medical transcription services ensure that this information is recorded and transcribed accurately and is easily accessible to all healthcare professionals involved in the patient’s care.
Accurate medical records are essential for providing high-quality patient care as they contain important information about a patient’s medical history, diagnoses, treatments, and progress. Medical transcription reports come in various types, each serving a specific purpose. These reports serve as a crucial part of the patient’s medical record. They ensure that accurate and complete medical records are maintained, facilitate communication between healthcare professionals, reduce errors, and improve the overall efficiency of the healthcare system.
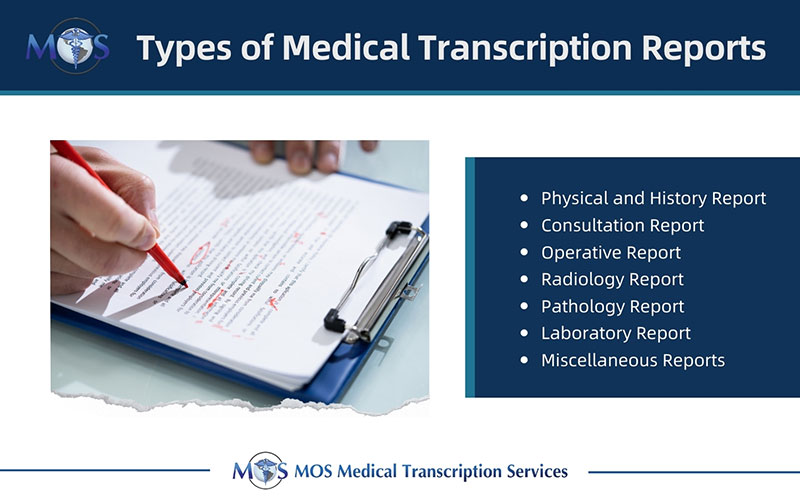
Different Types of Medical Transcription Reports
Medical transcription reports provide a comprehensive record of a patient’s care. They are used to track a patient’s progress, identify any issues or concerns, and ensure that the patient receives the best possible care. These reports may be used to support claims or to defend against medical malpractice lawsuits. Here are the different types of medical transcription reports:
- Physical and History Report: When a patient is admitted to the hospital, the admitting doctor or a resident typically orders this report. Usually, the main complaint comes first. The term “history” refers to the past medical history, social history, family medical history, and history of the current sickness. System reviews and a thorough physical examination from head to toe are typical. The report typically concludes with the patient’s treatment plan and the admission diagnosis.
- Consultation Report: Usually, a doctor who was referred to by the admitting doctor to treat the patient will write this report. As a result, the consulting physician typically has a different area of expertise than the admitting physician. For a second opinion, consultations are occasionally requested. Depending on the exact kind of consultation required, consultation reports typically include a succinct description of the patient’s disease and a specific physical examination. Also, the report might contain laboratory or x-ray results. The report often concludes with the consulting doctor’s assessment and treatment recommendations, and occasionally with a statement in which the consulting doctor expresses gratitude to the admitting doctor for the referral.
For information on transcription of consultation reports, read our blog post: Consultation Reports in Medical Transcription
- Operative Report: This report, which is being dictated by the operating physician, contains specific details about an operation and its procedure. Preoperative and postoperative diagnoses, the kind of surgery (or surgeries) that were performed, the names of the surgeon and the attending nursing staff, the kind of anesthesia and the name of the anesthesiologist, and a thorough description of the surgical procedure itself are all included in this report. Information on instrument counts, sponge counts, and blood loss are also determined by the surgical procedure. The report will frequently conclude with a disposition, the location to which the patient was taken after he left the operating room (typically the recovery room), and the patient’s state at that time.
- Radiology Report: Following a diagnostic procedure, the radiologist writes a report that incorporates his or her observations and impressions. X-rays, CT scans, MRI scans, nuclear medicine treatments, and fluoroscopic examinations are some examples of radiology reports.
- Pathology Report: This pathologist-written report summarizes the results of a tissue sample. The report’s main emphasis is on the sample’s microscopic findings and pathological diagnosis.
- Laboratory Report: This report details the results of tests done on biological fluids like blood and urine. Rarely are laboratory reports dictated separately; instead, they are frequently part of the H&P, consultation, or discharge summary.
- Miscellaneous Report: It includes reports from various hospital procedures like autopsies, electrophysiological tests, phacoemulsification, cardiac catheterizations, and psychiatric evaluations.
Healthcare providers are better equipped to provide comprehensive care when they have access to complete and accurate medical transcription reports. Choosing reliable medical transcription services can ensure that every single piece of information is documented accurately and in fast turnaround time.