Table of Contents
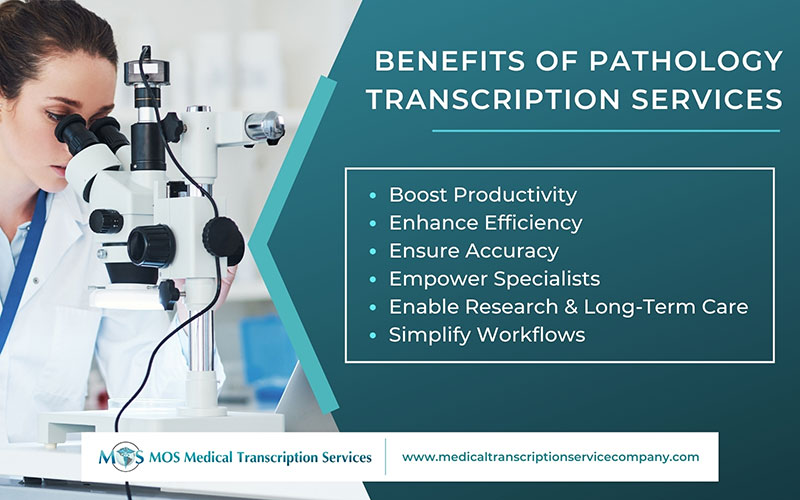
In modern healthcare, the right pathology transcription provider plays a quiet but critical role. Pathologists generate a high volume of dictations, ranging from descriptions of specimens to microscopic findings and final diagnostic impressions. Turning these spoken notes into precise, searchable medical records requires not just transcription skills, but also deep familiarity with the specialized terminology and workflows of pathology.
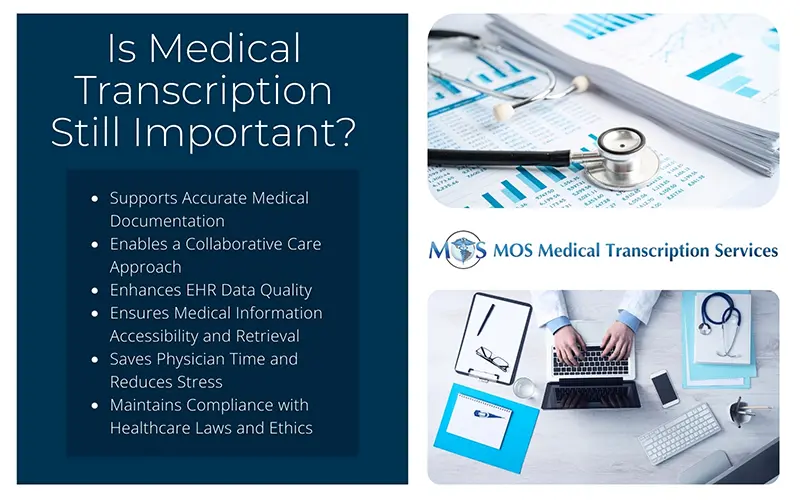
Unlike general medical transcription, pathology transcription demands heightened attention to detail. A misplaced word or number in a biopsy report can alter a diagnosis and affect treatment decisions. Choosing the right medical transcription services provider is a strategic decision that impacts accuracy, compliance, workflow efficiency, and ultimately, patient care.
So how do you select the right partner? Let’s explore the key criteria for choosing a pathology transcription provider.
7 Key Criteria to Choose the Right Pathology Transcription Provider
- 1. Accuracy Isn’t Just a Metric, it’s a Lifeline
Every transcription company claims high accuracy, but in pathology, “close enough” is never acceptable. Reports often contain technical descriptions, specimen identifiers, and clinical correlations that must be captured verbatim. An error here isn’t just clerical, it can undermine trust in lab results or even misinform treatment planning.Look for providers who:
- Guarantee accuracy levels of 99% or higher, backed by human transcription rather than AI alone.
- Employ specialized transcription services for pathologists who are trained in pathology terms (cytology, histopathology, hematology, molecular studies, etc.).
- Have multi-layer quality checks, ensuring one transcriptionist’s work is validated by another.
Accuracy in pathology isn’t about perfectionism, it’s about safeguarding diagnostic integrity and ensuring accurate and secure pathology transcription for healthcare.
- 2. Speed Without Compromising Quality
Pathology reports often feed into time-sensitive decisions-whether it’s confirming a cancer diagnosis or determining whether a surgery proceeds as planned. That means turnaround time (TAT) is just as critical as accuracy.The best pathology transcription providers offer:
- Flexible TATs ranging from a few hours for STAT cases to 24 hours for routine reports.
- A balance between speed and quality, ensuring urgent reports don’t bypass quality assurance protocols.
- Transparent communication about realistic delivery times, so clinicians aren’t left guessing.
In short, pathology transcription services with fast turnaround time can help clinicians make timely, life-saving decisions.
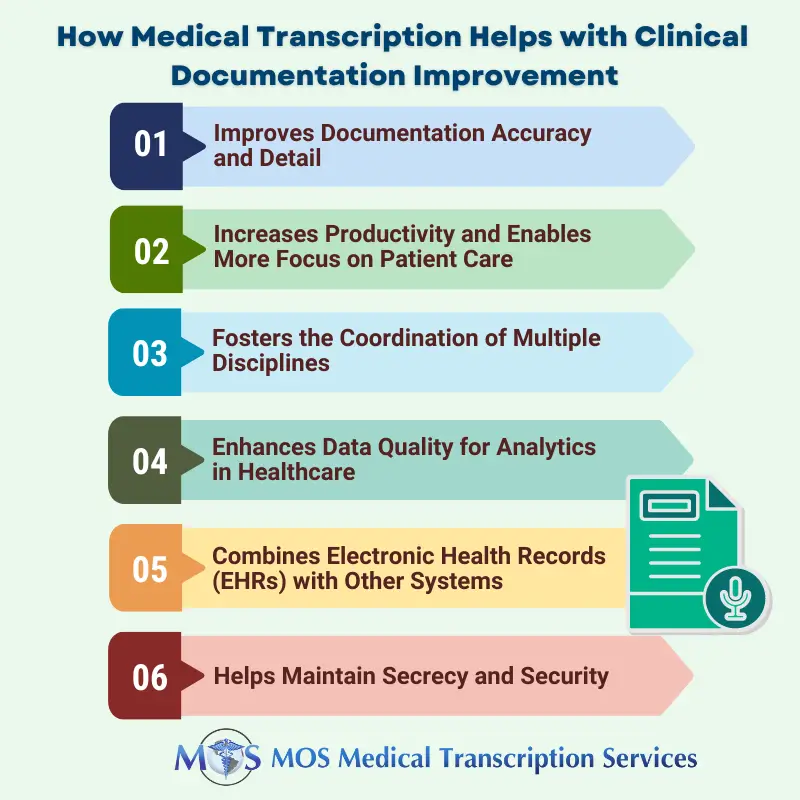
- 3. Expertise in Pathology-Specific Workflows
Pathology is not just another medical specialty; it has its own rhythm, lexicon, and documentation style. Generic transcriptionists may stumble over terms like “eosinophilic cytoplasm” or “immunohistochemical staining,” slowing workflows and inviting errors.When evaluating providers, consider:
- Do they have dedicated pathology transcriptionists with proven experience?
- Are transcriptionists trained to understand dictation formats unique to pathology reports (gross description, microscopic description, and diagnosis sections)?
- Can they adapt to different lab information systems (LIS) or integrate seamlessly with existing electronic health records (EHR)?
The more specialized the provider, the smoother the collaboration.
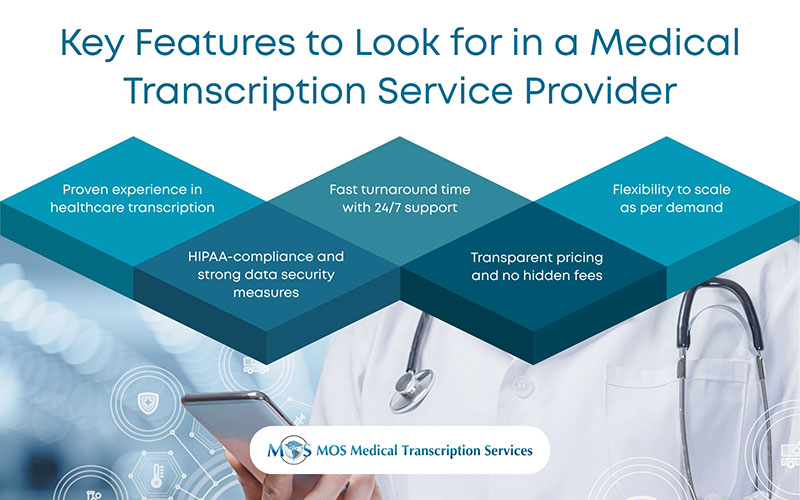
- 4. Security and Compliance: Beyond HIPAA
As pathology reports contain highly sensitive patient information, compliance isn’t optional, it’s foundational. But “HIPAA-compliant” is the bare minimum. A truly reliable pathology transcription provider should demonstrate a culture of data security.
Look for providers who:- Use end-to-end encryption (both in transit and at rest).
- Maintain secure VPNs and dedicated servers for healthcare clients.
- Conduct regular employee background checks and enforce strict NDAs.
- Offer audit trails so clients can monitor who accessed or edited a transcript.
HIPAA-compliant transcription is the minimum expectation, not the ceiling. True partners prioritize data confidentiality at every step.
- 5. Flexibility and Scalability
Pathology labs aren’t static. Case volumes can spike during flu season, after community health drives, or when new services (like molecular testing) are added. A transcription partner should scale with these changes without compromising quality or cost-effectiveness.
Ask yourself:- Can the provider handle surges in volume without delaying reports?
- Do they offer customizable transcription solutions tailored to your lab’s workflow?
- Are they open to both short-term projects and long-term partnerships?
Scalability ensures you’re not outgrowing your provider just when demand rises.
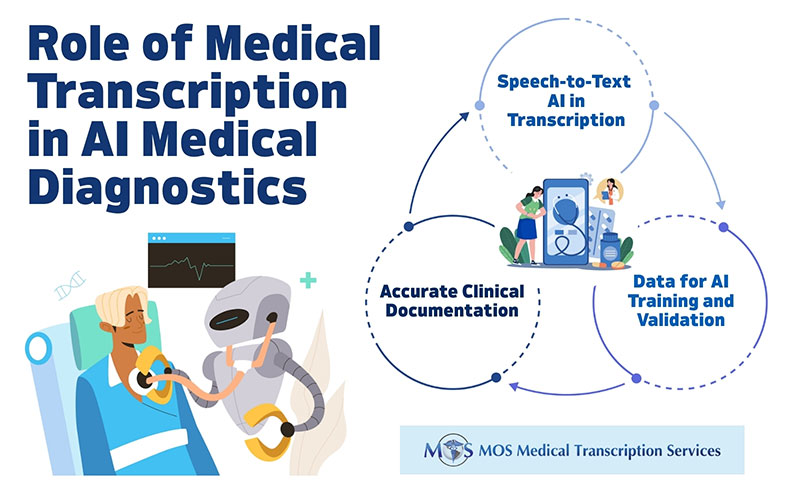
- 6. Human Touch vs. Technology: Finding the Right Balance
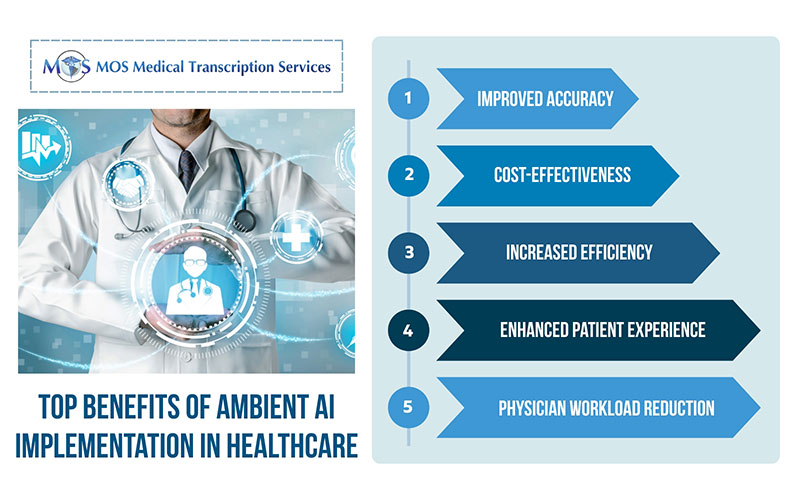
AI-driven transcription software has advanced, but in pathology, nuance matters too much to rely on automation alone. Automated systems often misinterpret complex terminology or struggle with accents and audio quality.The ideal provider strikes a balance:
- Using technology to assist transcriptionists (e.g., for formatting, time-stamping, or template management).
- Relying on human expertise for final review and correction, especially for pathology jargon.
- Offering editing services for clients who still use in-house dictation software but want transcripts polished by experts.
This hybrid approach combines efficiency with reliability.
- 7. Transparency and Client Support
A good provider isn’t just a vendor, they’re a partner. Pathology practices benefit from transcriptionists who understand their needs, provide ongoing support, and communicate openly.Key questions to ask:
- Do they provide clear pricing models (per line, per report, or subscription)?
- Can they offer client references or case studies specific to outsourced pathology reports?
- Is customer support available 24/7 to handle urgent issues?
Transparent communication and reliable support can save labs from workflow disruptions.
Choose Precision, Not Just a Provider
Pathology transcription is too critical to rely on a generic medical transcription service. The right partner goes beyond simply typing dictated notes—they enhance the efficiency, security, and reliability of your pathology practice.
When evaluating providers, prioritize accuracy, speed, expertise, compliance, scalability, and support. A provider who checks these boxes doesn’t just deliver transcripts; they safeguard diagnostic integrity and free pathologists to focus on what matters most-delivering timely, accurate diagnoses for patients.
Choosing wisely today means fewer errors, smoother workflows, and more confidence in every report tomorrow. With the right medical transcription services in place, pathologists can spend less time on documentation and more time delivering life-saving insights.