
Medical records are a combination of both self-reported patient information and the physician’s notes on diagnosis, care and treatment given to the patient. Complete and accurate patient record documentation is necessary to promote quality and continuity of care. It also supports proper claims payment when you completely and correctly document the services you provide. That’s why accuracy and reliability are the main features to look for in your medical transcription services provider. By enabling communication between providers, proper documentation supports patient safety, preventive health services, treatment, planning, and delivery of care.
Table of Contents
Electronic medical records (EMRs) tell the story of each patient’s medical condition—their diagnosis, the treatment they’ve received, and the physicians who saw them. They include physician notes, X-rays, test results, immunization reports, and other important medical documents and information. Ensuring accuracy in medical records requires effort on the part of healthcare providers across the board.
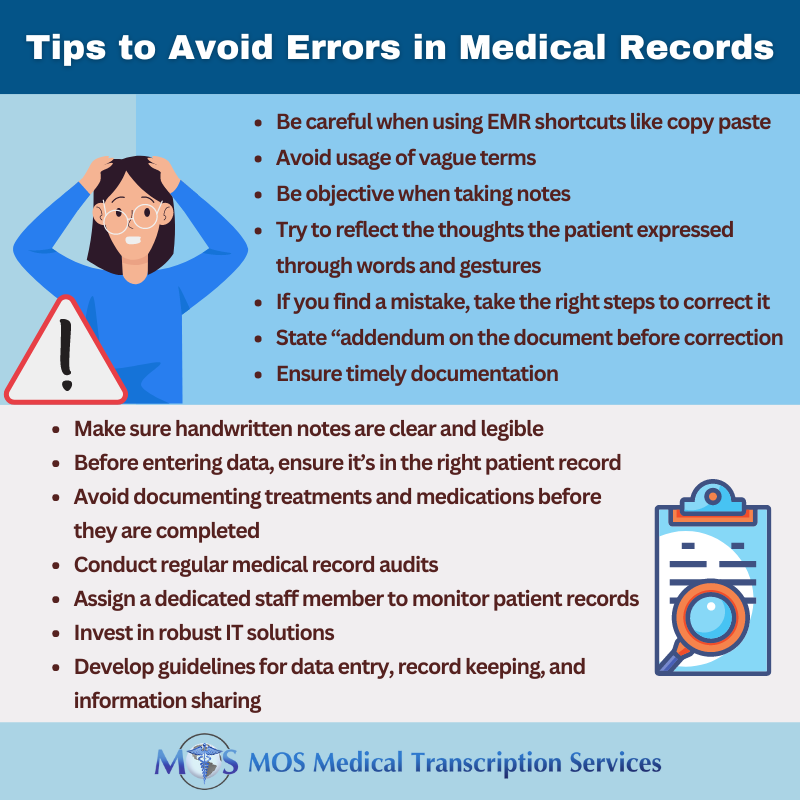
Here are some best practices to help ensure accuracy in medical documentation and avoid errors.
Medical Record Documentation Best Practices
1. Keep a unique, individual record for each patient
Each file should include:
- Patient demographic information–the patient’s name, birth date, and social security number.
- Medical history-past diagnoses, treatments and medical care, and allergies, if any.
- Medications-what medications the patient is taking, what medicines work and don’t work, and what might cause an allergic reaction.
2. Ensure clarity
Although EMRs are the norm, documentation can be handwritten by the physician or the nurse and scanned into the record. Handwritten notes should be legible and easy to read. If there’s anything that lacks clarity, take steps to correct it. For example, if there is a mistake on a handwritten note, cross it out with a single line and enter the correct information. Don’t scribble over the erroneous text or use whiteout. Add an amendment to correct a mistake in the EMR.
3. Watch out for charting errors
Make sure medical history and medication instructions are entered correctly.
Medical errors that lead to unreliable healthcare documentation include:
- Incomplete or missing data
- Unnecessary blank space in forms within the medical records
- Misplaced medical documentation
- Not entering new medical conditions or symptoms
- Misuse of copy and paste function in the EHR
- Errors due to illegible physician’s handwriting or misunderstood dictation
- Entry in wrong charts of files
- Duplication of medical records
- Failure to document omitted treatments/medications
In a patient survey study published in in 2020, 1 in 5 patients who read a note reported finding a mistake and 40% considered the mistake serious. Even small errors or omissions in a patient’s medical record can have grave consequences and cause patient harm with legal consequences for your practice. For example, if an order is illegible, a patient could get the wrong medication, test, item or service which could put their health and safety at serious risk.
4. Ensure organized record-keeping
Make sure all documents are organized in chronological order and easily retrievable for review and available for use at each patient visit or whenever needed. Each office visit should be recorded separately – don’t copy paste in electronic medical records. Ensure that both paper and electronic patient records are secure and accessible only to authorized individuals.
5.Maintain comprehensive documentation
Provide comprehensive health information about the patient – keep in mind that “if it isn’t written down, you didn’t do it. Provide as much detail as possible so that the next physician seeing the patient will know exactly what the patient was being treated for, including the future plan of action.
6. Use standardized terminology
Natural language allows for rich expressiveness but create ambiguity and a lack of standardization in EHRs To ensure consistency and minimize ambiguity, use standardized medical terminology. Resources that contain standardized medical terminology include SNOMED CT (Systematized Nomenclature of Medicine Clinical Terms), Logical Observation Identifiers Names and Codes (LOINC), and the International Statistical Classification of Diseases and Related Health Problems (ICD). Using standardized language improves interoperability between different systems and applications, and reduces risk of miscommunication and errors in clinical decision-making.
7. Sign Healthcare Record Notes
Every note entered into the EMR, including electronic notes, should be signed and dated. Include a digital signature and stamp with the date. If there is unused space on a signature line, draw a single solid line across the remaining space. This helps prevent unauthorized modifications of the signature or other documentation.
If dictated notes are transcribed by a third party, review them for transcription errors and ensure that entries are signed before they are added to the patient’s record.
Outsource Medical Transcription to an Expert
If you outsource medical transcription, the importance of partnering with a reliable service provider cannot be overstated. Errors in medical documentation and transcription can have a far-reaching impact, affecting patient safety and care across the continuum.
A 2020 JAMA study compared 105 encounter notes or transcripts to audio recordings from 36 physicians to identify discrepancies. The researchers found 636 documentation errors, including 181 charted findings that did not take place, and 455 findings that were not charted. Ninety percent of notes contained at least 1 error.
Key considerations when choose a medical transcription company include:
- Make sure that the company can provide quality transcripts. Ask about their QA measures and what guarantees they offer.
- Ensure that their team is well qualified and can successfully understand various accents and ESL physicians or dictators. Leading companies offer prospective clients a free trial to help them make an informed decision.
On your part, make sure your dictation is clear. For good audio recording, speak in a normal tone, ensure proper mic placement, and choose a quiet environment. Be extra careful when using similar sounding words that can create confusion or lead to spelling mistakes (for example, perfusion/profusion; cord/chord).
Experienced transcriptionists will verify the transcript while listening to the audio recording. They will look for each element in the transcript in the corresponding physician’s note, to see whether it is present, missing or inaccurate, and make the necessary corrections. Partnering with a HIPAA complaint medical transcription company will ensure that all healthcare data you entrust them with remains secure and confidential.


