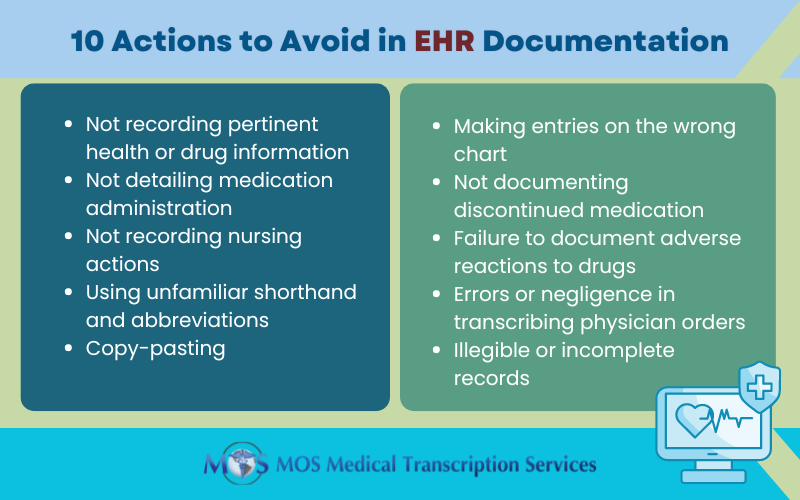
Electronic health record (EHR) systems serve as powerful technology platforms for data collection on office visits, diagnoses, treatments, and prescriptions, and medical transcription outsourcing helps physicians ensure accurate EHR documentation. EHR data is widely used for research and to study issues in clinical medicine such as medical overuse. Overuse of medical care or subjecting a patient to unnecessary care is a costly and pervasive problem in the United States.

What is “overuse of medical care”?
The Lown Institute defines overuse as “catchall term for medical tests, treatments, and other services that patients don’t need or don’t want”. Instances of overuse of medical care are:
- When a patient is hospitalized unnecessarily – the treatment is very unlikely to benefit the patient because there is no evidence of the disease or symptom to diagnose or treat, or because the potential risks of treatment are greater than the possible benefits.
- If the patient receives a test, treatment, drug, or procedure that is unnecessary, ineffective, or unwanted. “Ineffective” means the treatment makes no difference to the patient’s condition and “unwanted” means that, if fully informed, the patient would choose another testing or treatment option.
- Overdiagnosis, where patients are diagnosed with conditions that were unlikely to cause symptoms or shorten life.
According to an August 2018 Dark Daily report, a Washington State healthcare watchdog organization maintains that “wasteful” spending for “low-value” clinical laboratory tests and other procedures amounted to a whopping $282-million in a single year. The report also presents the results of a Washington Health Alliance (WHA) study “First, Do No Harm: Calculating Health Care Waste in Washington State,” on medical overuse over the period July 2015 and June 2016 on 1.3 million patients who had one of 47 procedures or tests that the US Preventive Services Task Force had labeled as overused:
- More than 45% of the healthcare services examined are determined to be “low value” since they offer little benefit in certain clinical scenarios.
- 47.9% of patients had a low-value test or procedure that was unnecessary.
- An estimated $282 million (36% of spending) was wasted on low-value services.
- 11 common tests, procedures, and treatments such as preoperative tests, laboratory studies prior to surgery, and too frequent cancer screenings account for 93% of low-value services and 89% of the estimated wasted spending.
Common Examples of Overused Medical Procedures
According to the WHA study, the most overused low-value services are:
- Too frequent cervical cancer screening in women
- Preoperative baseline laboratory studies before low-risk surgery
- Unnecessary imaging for eye disease
- Annual EKGs or cardiac screening in low-risk, asymptomatic individuals
- Prescribing antibiotics for acute upper respiratory and ear infections
- PSA (prostate specific antigen) screening
- Population-based screening for 25(OH)-D deficiency
- Imaging for uncomplicated low back pain in the first six weeks
- Preoperative EKG, chest x-ray, and pulmonary function testing prior to low-risk surgery
- Cardiac stress testing
- Imaging for uncomplicated headache
Participants in a National Summit on Overuse convened in September 2012 in Chicago identified five treatments as overused: use of antibiotics for viral upper respiratory infections; over-transfusion of red blood cells; tympanostomy tubes for middle ear effusion for brief periods; early scheduled births without medical need; and elective percutaneous coronary intervention.
Why does medical overuse occur?
Physicians generally make well-informed treatment decisions based on clinical evidence and expertise, but choices may be also driven by other factors such as economic incentives, fear of liability, worry about uncertainty, habit, and hunches. On their part, many patients tend to believe that more health care is better, and are not accepting of recommendations that seem to limit choice or of advice to wait to see whether a symptom improves. For instance, a Propublica report notes that patients’ mindset contributes to overuse of medical care. Patients often insist that their healthcare provider write a prescription or perform a test, which has led to problems like the overuse of antibiotics.
How can the problem be tackled?
Physicians and patients must work together to minimize waste in health care. In 2012, the American Board of Internal Medicine Foundation launched the Choosing Wisely campaign to encourage doctors and patients to discuss the issue of unnecessary tests and treatments. The Choosing Wisely campaign makes a difference by focusing on the following aspects, according to a Harvard Business Review report:
Putting quantity in the context of quality: The campaign focuses on making patients and physicians see that more care is not always better care. Patients are about why an unnecessary test could be detrimental to them so that doctors and patients can have more constructive conversations about the tests. The campaign also looks to change the way many doctors practice by avoiding ordering of unnecessary prescriptions and tests.
Changing how quality is managed: This involves putting in place a quality management system which helps providers and patients make better decisions about when care is necessary or improper. For example, new heart disease prevention guidelines use a personalized assessment that helps physicians detect a patient’s risk for a heart attack and whether the patient should take a cholesterol-lowering statin drug as well as its dose.
Guiding physicians about reconsidering the value of their services: Many physicians tend to orders unnecessary tests at least once per week due to fear of lawsuits and general clinical uncertainty. One important goal of Choosing Wisely is to educate physicians that not ordering unnecessary services can have as much value for patients as ordering appropriate tests and treatments.
The Choosing Wisely campaign recommends that patients ask their physician five basic questions before undergoing any test or treatment:
- Do I really need this test or procedure?
- What are the risks and side effects?
- Are there simpler, safer options?
- What happens if I don’t do anything?
- How much does it cost, and will my insurance pay for it?
The WHA believes the shift from fee-for-service healthcare to value-based reimbursement models can provide a solution to overuse. The WHA report states: “We need to keep our collective ‘foot on the gas’ to transition from paying for volume to paying for value in healthcare.” It also proposes value-based provider contracts should include measures of overuse and not just measures of access and underuse.
Medical care overuse is the subject of active research. A study published in the Journal of the American Medical Association (JAMA) in 2017 reported that EHRs have the potential to decrease overuse of low-value care by allowing for better data collection and direct intervention. Medical transcription companies play an important role in ensuring error-free medical records to support research applications as well as provision of quality care.







![Tips for Patients and Physicians to Optimize the Office Visit [Infographics]](https://www.medicaltranscriptionservicecompany.com/wp-content/uploads/2020/01/tips-patients-physicians-optimize-office-visit.jpg)
