Table of Contents
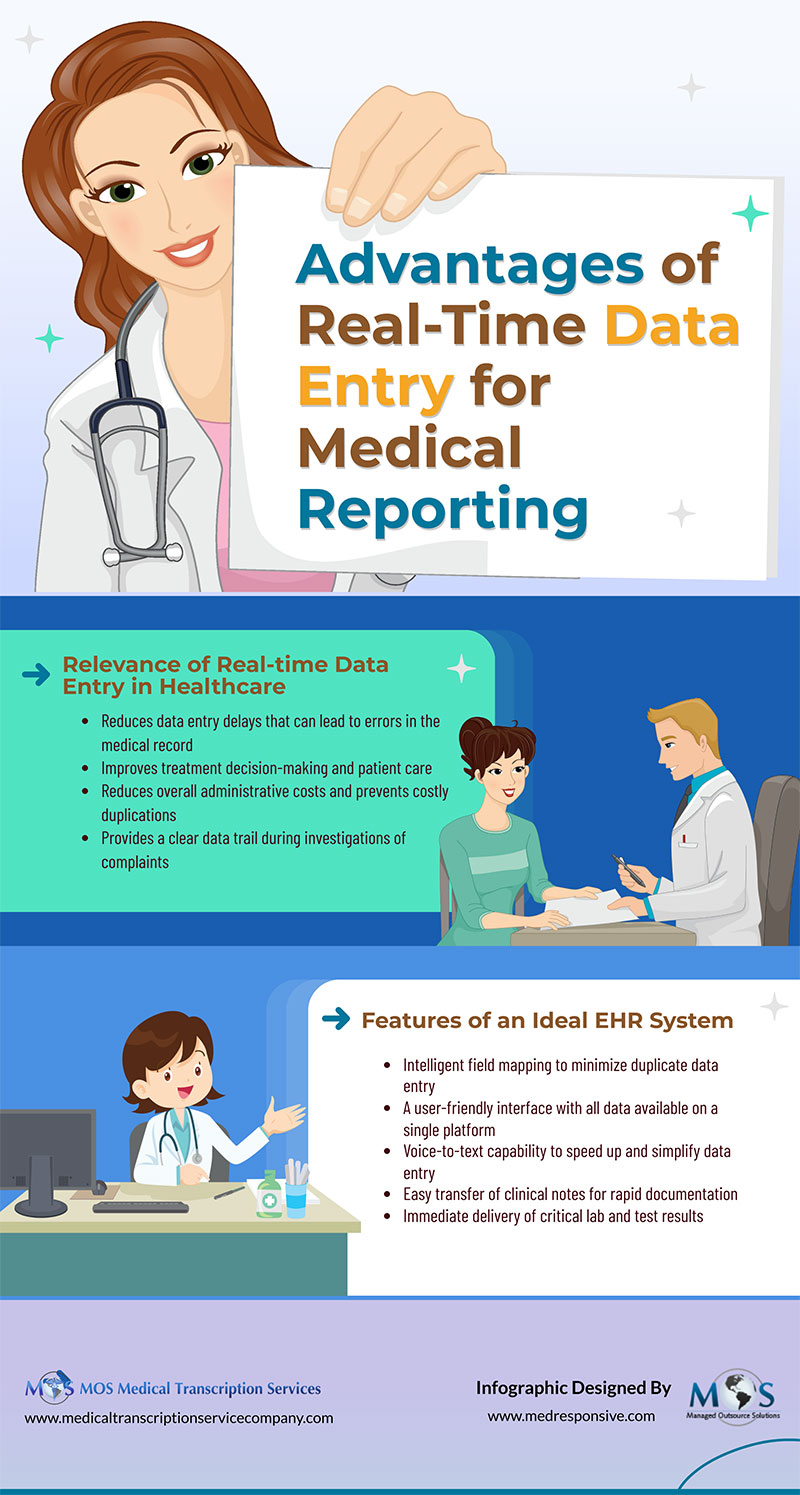
Medical transcription is all about converting audio recordings of physicians’ handwritten medical notes into text. Medical transcription is still important in the healthcare sector today, despite technological advancements and the introduction of electronic health records (EHRs). This is mostly due to the significance of accuracy in medical documentation. Medical transcriptionists are taught how to comprehend complicated medical jargon, distinguish different accents, and ensure that the final product is error-free. In medical settings, where errors can have major effects on patient care, this level of precision is crucial. Additionally, medical transcription frees up doctors’ and other healthcare workers’ time so they can concentrate on patient care rather than on menial tasks such as documentation. Healthcare providers can streamline their processes and boost overall effectiveness by outsourcing medical transcription.
Importance of Medical Transcription Even Today
There are many developments happening in the healthcare sector. One such change that has occurred over the past few years is the demand for medical transcriptionists. Medical transcriptionists are in greater demand as a result of the numerous changes that the healthcare sector is going through. The demand for this occupation has increased recently as more and more people turn to technology for assistance. Over time, the trends in the healthcare sector have changed, and more regulations have been put in place that have an impact on the jobs of medical transcriptionists. Nevertheless, despite the shifting environment, there is still a need for these professionals.
Reasons Why Medical Transcription Is Still Relevant
- Life-saving communication: In the course of their lifetime, patients experience a variety of ailments and receive care and treatment from numerous hospitals, clinics, and physicians. Their past medical history can be shared with medical professionals more effectively if a detailed and accurate record is kept. Patients frequently forget important information regarding previous diseases and diagnoses. But medical professionals are aware of the impact a patient’s medical history has on the course of their illness and their response to treatment. These crucial bits of information are preserved by medical transcription so they can be disseminated among many medical professionals and doctors in order to potentially save someone’s life.
- A requirement for support workforce: A doctor’s knowledge unquestionably determines how a patient will be treated. However, a larger healthcare staff is involved in patient care.
By using medical transcription and maintaining a record of a patient, you not only make the work of associated healthcare practitioners easier, but you also give them crucial information to tailor the patient’s care regimen to their needs. Medical transcription will give the supporting staff reliable information as opposed to relying on the patient and the patient’s kin’s word of mouth or waiting for the doctor to be available.
- Faster diagnosis: Medical transcription also aids in the quicker diagnosis of disease by maintaining records and histories. Doctors and other healthcare professionals do not need to be reminded of this. Medical transcription will give doctors all the records, large or small, they need to review while making a diagnosis. Significance of appropriate diagnosis is well known and one incorrect medical procedure or drug prescription can be lethal and ruin a doctor’s reputation and professional future. A professionally edited medical transcript can almost completely eliminate these chances.
- Legal safety net: Although it is uncommon, there is always a risk that a sick patient, her family, or the family of a deceased patient will approach the judiciary if they suspect some malpractice during treatment. In the event of such a bad thing happening, doctors need a safety net. In accordance with HIPAA (Health Insurance Portability and Accountability Act), retaining records has become crucial to the delivery of healthcare. The care they are giving to a patient now requires doctors to create comprehensive records about it. Medical transcription is done in accordance with HIPAA regulations.
- Assist patient insurance claims: Many patients rely on insurance funds for their medical expenses. It is painful to see a patient forgo necessary care because of the high expense or because a treatment is too expensive for them. The hospital billing staff can utilize the patient record they created after transcribing the data to submit it to the insurance companies for claim settlement. Verifying medical data is a crucial step in the medical insurance claim settlement process. The most trustworthy papers or files to use for that purpose are transcripts. These medical transcripts may also be used as proof in court if there is a dispute over payment of claims between patients and insurance companies.
The Future of Medical Transcription
Today’s world is expected to continue moving toward technology-based solutions, which will likely have an impact on the future of medical transcription. Transcribing medical reports and notes is becoming simpler and quicker because of developments in speech recognition technology and artificial intelligence (AI). Although these technologies can boost productivity, they cannot take the place of the human knowledge and meticulousness that medical transcriptionists offer. As a result, it is anticipated that a hybrid strategy that combines automatic transcription with human editing and review would gain popularity.
A similar shift toward patient-centered treatment is what will shape medical transcription in the future. Prioritizing brief, intelligible, and clear communication with patients will be essential for healthcare practitioners as they work to enhance the patient experience. Providing accurate and readily available medical reports and records falls under this category. Thus, in order to ensure that the information they transcribe is patient-friendly and easily understandable, medical transcriptionists may need to adapt to new standards and requirements, and therefore outsourcing medical transcription is still relevant.