Pathology reports are an essential source of information for healthcare documentation, helping to diagnose and treat patients. For the sake of accuracy and patient care, these reports must be transcribed quickly and accurately. Therefore, in order to maintain high quality and precision, it is ideal that providers of professional medical transcription services perform pathology transcription.
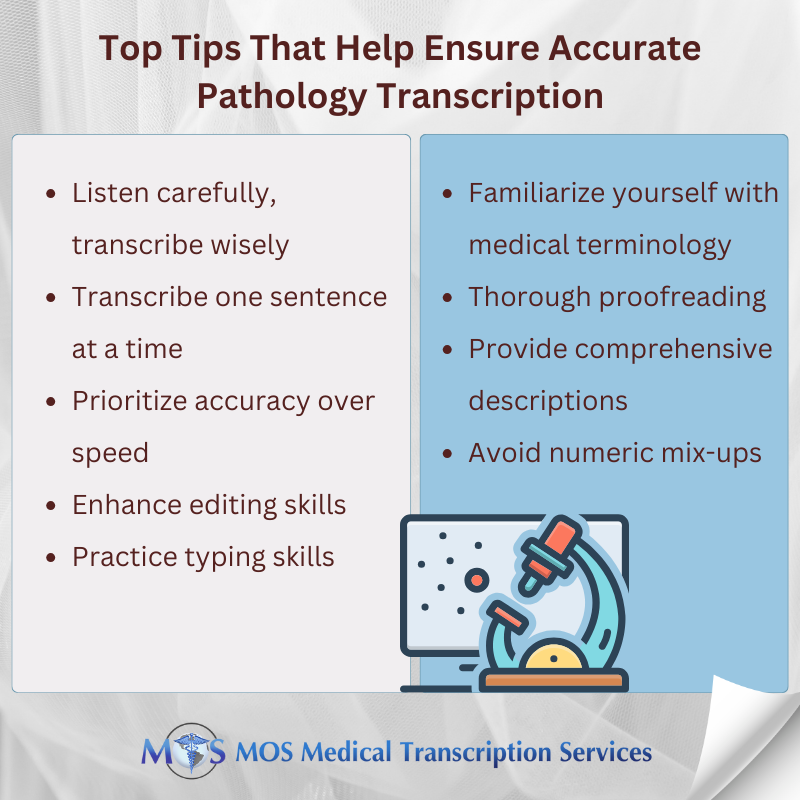
Let us consider some of the best tips that professional transcriptionists follow to ensure accurate transcripts of the audio material.
Pathology Transcription – Best Practices to Follow
It involves converting dictated or audio pathology reports into text format. This is done to make it easier to save and retrieve the information electronically. Transcription of pathology records can be performed manually or with the aid of software.
The quality of medical care depends on accurate transcription of physicians’ notes, and the safety of the patient depends on the quality of care. If the medical transcription contains mistakes, the hospital will have to invest significant time in fixing the transcription. As a result, transcription professionals need to improve their abilities to provide accurate, dependable, and speedy transcription.
Here are some best steps that professional transcriptionists take to ensure accurate pathology transcription. These may prove useful to your transcription team if you are handling pathology transcription in-house.
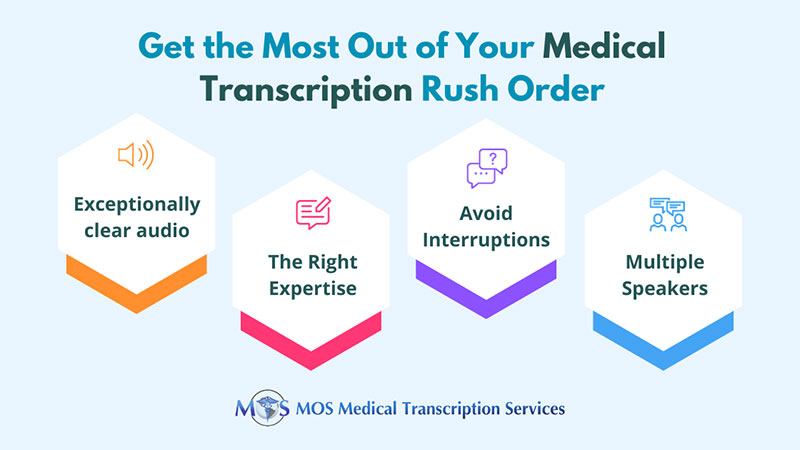
- Listen carefully, transcribe wisely: Avoid the common mistake of transcribing while listening simultaneously. Take the time to listen to the audio first, ensuring you have a clear understanding of the recordings before starting transcription. This approach significantly reduces errors and enhances accuracy.
- Transcribe one sentence at a time: Break down the transcription process by focusing on one sentence at a time. This method helps maintain context awareness and reduces the chances of discrepancies in the report.
- Prioritize accuracy over speed: While speed is valuable, accuracy should never be compromised. Strive for precision in transcription to minimize typos and ensure the integrity of the pathology report. Utilize transcription tools and software to improve accuracy without sacrificing speed.
- Enhance editing skills: Editing plays a vital role in ensuring the correctness of the transcription. Continuously hone your editing skills to rectify spelling, syntactic, and grammatical errors effectively.
- Practice typing skills: Enhance typing speed and accuracy through regular practice. Utilize all fingers while typing and seek guidance from experts to determine the most efficient typing technique for you.
- Familiarize yourself with medical terminology: Acquaint yourself with frequently occurring medical terms to ease the transcription process. Understanding context-specific abbreviations and medical jargon enhances transcription accuracy.
- Thorough proofreading: Develop proficient proofreading skills to quickly identify and correct critical errors in the transcript. Pay close attention to medical terminology, diagnoses, and dosage information during the proofreading process.
- Provide comprehensive descriptions: Supplement pathology reports with additional information, including accurate dosage units and pertinent details. Clear and concise descriptions facilitate better understanding by healthcare professionals.
- Avoid numeric mix-ups: Exercise caution when transcribing numeric values, particularly in dosage amounts. Ensure precision in recording numeric data to prevent errors in prescription drug information.
Learn about the challenges of pathology transcription and how to overcome it from our blog post Navigating the Challenges of Pathology Transcription: Solutions for Success
Ensuring Error-free Transcripts with Expert Pathology Transcription
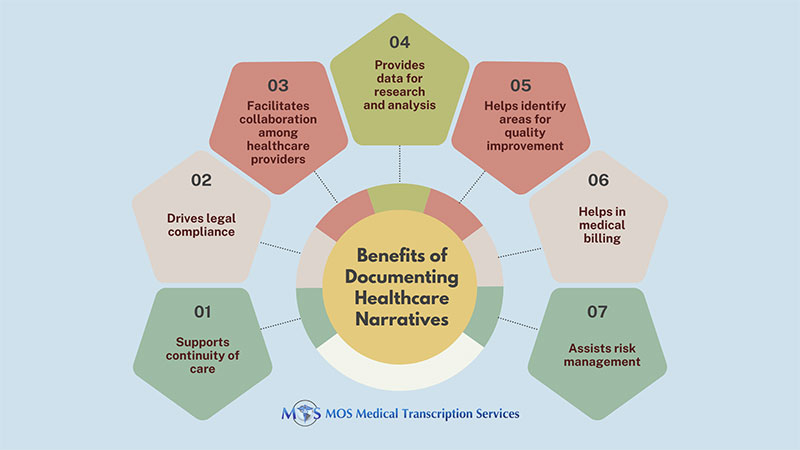
Precise pathology transcription forms the basis for accurate pathology reports, which is an essential tool in contemporary medicine for accurate patient diagnosis and treatment. Treatment regimens, patient care techniques, and important medical choices are based on these reports.
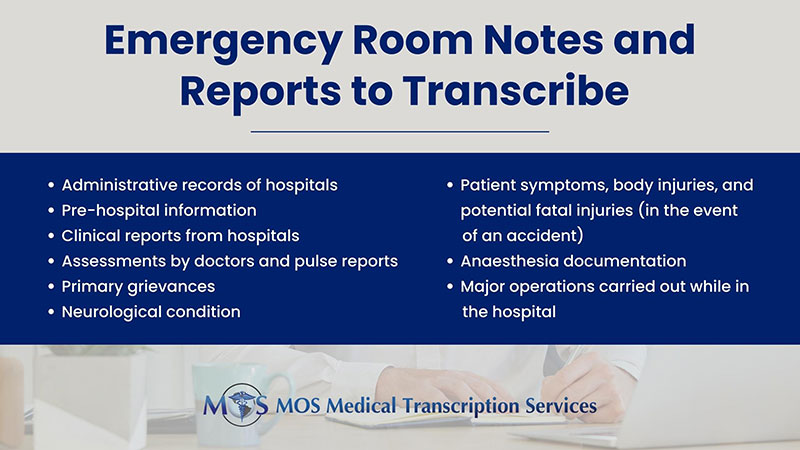
A pathology report has the following components:
- The patient’s name and individual identifiers. These include Social Security number, patient ID number, and date of birth.
- A case number which serves as the particular specimen’s identification.
- The time and type of procedure (such as a blood sample, surgery, or biopsy) used to get the specimen
- The patient’s past health and the clinical condition he/she has right now
- An overview of the specimen that was received by the laboratory
- A thorough account of the pathologist’s observations made when examining the specimen under a microscope
- Ultimately, the diagnosis is the “bottom line” of the testing procedure. To determine the best course of treatment, the treating physician considers the final diagnosis
- The pathologist’s name, signature, and pathology lab’s address are all included
By faithfully transcribing pathology findings, transcribers play a vital role in ensuring the accuracy, reliability, and clinical utility of pathology reports, ultimately contributing to improved patient outcomes, enhanced patient safety, and effective healthcare delivery.
A reliable provider of pathology transcription services helps in generating error-free pathology transcripts that healthcare professionals can use to provide the best treatment plan and quality patient care.