Table of Contents
Neurology is a medical specialty with unique documentation challenges. To provide safe and effective treatment, neurologists rely on reports of complex patient histories, sophisticated physical examinations requiring detailed motor and sensory evaluations, and specialized neurophysiological and imaging tests. But with their busy schedules, neurologists and their staff often find it challenging to maintain accurate and timely patient records. Neurology documentation challenges arise from the need to capture subtle neurological signs for complex, often chronic, conditions in the electronic health record (EHR), and comply with stringent billing and coding regulations, all while maintaining patient confidentiality and accuracy.
Errors and omissions in neurology records can compromise patient care, increasing potential for litigation. Let’s explore how EHR-integrated medical transcription services can help minimize the impact of the documentation burden on neurologists and patient care.
Limitations of EHR Systems in Neurology
EHRs are designed to manage patient data and clinical workflows. However, complex and non-intuitive interfaces make EHR data capture a challenging task in any specialty, increasing the time clinicians spend on entering information into the system.
Neurology EHR systems are specially designed for neurology practices, offering features like neurology-specific templates, integrated imaging viewers (MRI, CT, EEG), chronic disease tracking tools, and seamless interoperability with labs and other providers. They improve care by centralizing information, reducing risk of errors, and enhancing decision-making. However, the time-consuming nature of documentation and potential usability issues leads to increased provider burnout and reduced time for direct patient care.
The key challenges of neurology EHRs are:
- Documentation Burden: The time required to input detailed neurological assessments, including cranial nerve exams, reflexes, and motor/sensory evaluations, can impact time spent with patients.
- Usability and Interface: Some systems can be difficult to use, confusing, or not user-friendly. Even simple tasks such as entering notes, ordering labs, reviewing past records) may require multiple clicks or complicated navigation. The interface feels cluttered or non-logical, forcing providers to spend extra time learning or working around it, leading to frustration, burnout, and reduced efficiency for neurologists.
- Interoperability: Many systems present challenges in sharing patient data seamlessly between different EHR systems and institutions. This affects the way neurologists communicate, exchange, and use patient data seamlessly across organizations, providers, and platforms.
Ultimately, EHRs increase time spent on data entry by physicians. Studies have linked physician burnout in neurology to the documentation workload. A systematic review titled “Burnout in Practicing Neurologists: A Systematic Review and Meta-Analysis” found that among neurologists globally, about 65.9% report experiencing burnout. In the same meta-analysis and other neurology specialty surveys, “clerical work” and “amount of documentation” are named explicitly among the significant predictors of burnout risk. Tasks like EHR use, charting, and administrative paperwork are repeatedly mentioned (American Academy of Neurology: Neurology Resources).
Compliance and accuracy issues in standard EHR documentation arise from delayed entries, user errors like incorrect patient selection or unchecked drop-down menus, poorly designed user interfaces, and inadequate staff education on documentation best practices. These issues can compromise patient care, and result in billing problems, regulatory violations, and negative impacts on data integrity, affecting operational efficiency.
EHR Integrated medical transcription support can ensure accurate and timely digital patient records in neurology.
How EHR Integrated Medical Transcription Supports Neurologists
Neurology practices handle some of the most complex clinical documentation in medicine. From EEG and EMG interpretations to detailed evaluations for conditions like epilepsy, Parkinson’s disease, and neuropathies, neurologists must capture highly specialized information with precision.
Neurology documentation demands technical accuracy and extensive knowledge of subspecialty terminology. Without integration, neurologists can face issues such as duplicate data entry between transcription systems and the EHR, delays in updating test results and patient notes, and higher risk of errors that could impact diagnosis, treatment, and billing.
Managing these common documentation challenges faced by neurologists in the EHR can be time-consuming. Integrating neurology transcription services with EHR systems can dramatically improve workflow efficiency while supporting accuracy and compliance.
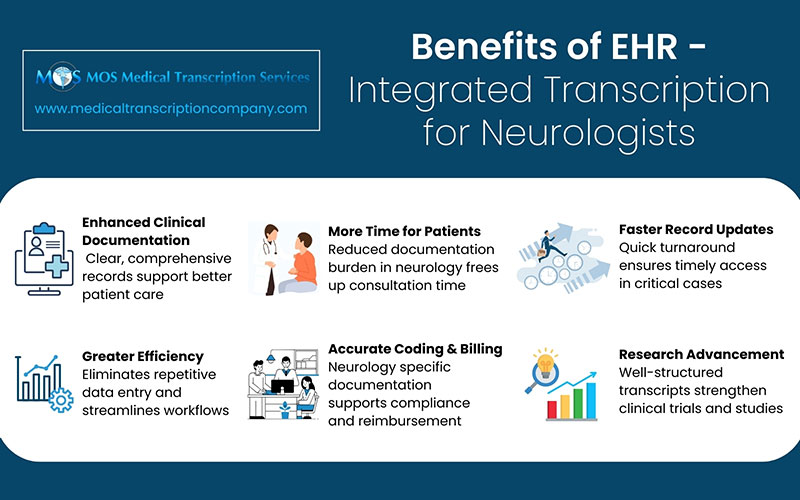
The benefits of EHR integrated transcription for neurology practices include:
Accurate Documentation
Neurologists can dictate EEG, EMG, and imaging interpretations directly into the EHR. Transcriptionists trained in neurology-specific language ensure precise recording of complex neurological tests (EEG, EMG, imaging) and conditions like epilepsy, Parkinson’s, and neuropathies, reducing errors that could affect diagnosis, treatment, billing, or compliance.
Faster Access to Clinical Data
EHR integration allows dictated notes and test findings to appear instantly in the patient’s record. This means neurologists and interdisciplinary teams can act quickly—critical when managing seizures, strokes, or other emergencies.
Reliable Neurology Records
AI-driven tools combined with human quality checks provide dependable HIPAA-compliant records, minimizing reduced medico-legal risks and supporting high standards of care. Automation eliminates the need to re-enter information for billing and coding. Properly documented records also support accurate claims, minimizing denials and ensuring compliance with neurology-specific billing guidelines.
Time Efficiency
Dictation allows neurologists to save time on documentation, focus more on patient care, consult more cases, and stay engaged in research and education. Quick transcription ensures updated, accurate patient records are available promptly, which is especially critical in emergencies.
Better Collaboration
Clear transcripts of diagnostic findings and treatment plans integrated seamlessly into the EHR allow neurologists, radiologists, primary care physicians, and other specialists to collaborate effectively. Such smooth communication supports both patient outcomes and research efforts.
Integrating medical transcription with EHRs helps neurologists overcome documentation challenges, reduce burnout, and deliver better patient outcomes. It ensures that complex neurological data is captured accurately, reduces administrative bottlenecks, and enables faster, more effective patient care. By partnering with a specialized medical transcription company, neurologists can ensure timely and accurate EHR-integrated clinical documentation into their workflows, reduce administrative burdens, improve efficiency, protect compliance, and enhance both clinical and research outcomes.