Electronic health record (EHR) debates can be contentious. While some praise EHR systems for enhancing the medical documentation process, others find the system burdensome. Contradictory findings are found in even studies on EHR’s impact on physician burnout rates and patient care. Medical transcription services can be helpful since they relieve healthcare practitioners of the stress of data entry during the patient visit, freeing them up to concentrate on providing high-quality care. These services can assist in resolving challenges with EHR use by ensure precise and prompt documentation of patient encounters.
Table of Contents
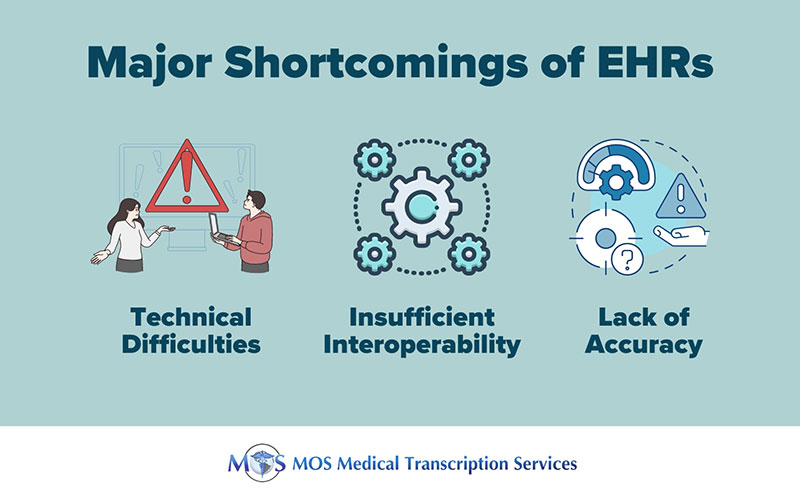
Shortcomings of EHRs
- Technical Difficulties: A medical facility’s reliance on EHRs could prove disastrous in the event of a technological issue. In order to diagnose a patient correctly, healthcare professionals consult their medical history. But their capacity to deliver optimal care may be compromised if the digital storage system breaks down. Furthermore, rather than accessing the files from the cloud, the attending physician will need to question the patient about their medical history. If technical glitch lasts several hours, it can result in delays and mistakes, compromising care.
- Insufficient Interoperability: Interoperability enables communication and collaboration, enhancing care. However, the majority of EHR systems prohibit the exchange of data. Absence of data exchange can improve system security, but it also reduces access to information needed to provide proper medical care.
- Lack of Accuracy: Many physicians copy and paste data within EHR system in order to save time. However, most of them may not have enough time to check every word or data point while copy-pasting lots of data, which can potentially result in proliferation of errors in the chart.
A study titled “A Qualitative Analysis of the Impact of Electronic Health Records (EHR) on Healthcare Quality and Safety” published on Sage Journals noted that EHRs had several disadvantages. The researchers surveyed physicians, hospitalists, nurse practitioners, nurses, and patient safety officers and listed their opinions on EHR implementation and use:
- While some nurses thought that using an EHR would increase efficiency, others thought that it would take a lot of time.
- Physicians, nurse practitioners, and patient safety officials emphasized how crucial EHRs are for preventing medical errors by making patient data more easily accessible and readable. Nurses, however, had reservations about the data’s accuracy.
- Given the lack of system integration, interoperability seemed to be a concern for medical professionals and patient safety officials.
Are you facing interoperability issues?
Read more: EHR Interoperability: Importance, Challenges and Solutions
Combining EHR and Transcription – A Practical Solution
As of 2021, nearly 9 in 10 (88%) of U.S. office-based physicians adopted any EHR and nearly 4 in 5 (78%) had adopted a certified EHR, according to HealthIT.gov. An approach that blends EHR and medical transcription is a practical solution to optimize EHR documentation.
In this system, physician dictations are transcribed with the help of transcriptionists and discrete reportable transcription (DRT) technology is used to populate the transcribed data within the EHR system. This helps them to take advantage of both structured templates and narrative description depending on the care settings and practice patterns. For example, structured history and physical templates populated by a physician assistant may be useful in the case of one care setting while transcribed narrative report may be the best for findings and assessments. If providers partner with a medical transcription company with a good quality assurance processes, they can ensure that data within the EHR is accurate and avoid errors associated with copy-pasted data. It can also help eliminate the need for stressful data entry by physicians and allow them to focus on what they do best – care for patients.


