Table of Contents
Rheumatologists diagnose and treat a wide range of autoimmune and musculoskeletal conditions, many of which are chronic and involve complex inflammation of the connective tissues, such as bones, joints, muscles, tendons, and ligaments. These conditions often present unique challenges in both diagnosis and management. Accurate and timely documentation is essential for maintaining continuity of care and ensuring regulatory compliance. Physicians’ notes must be transcribed with precision to avoid errors and ensure reliable patient records, which is why many healthcare providers turn to specialized medical transcription services. Partnering with a reliable company can save time and costs, allowing physicians to focus on patient care.
Let’s take a closer look at what exactly makes rheumatology transcription so complex and how outsourcing addresses these documentation challenges.
Unique Challenges of Rheumatology Transcription
Rheumatology transcription presents several unique challenges due to the complexity and specialized terminology of the field. Some of these challenges include:
Detailed Medical History and Records: Rheumatology assessments may involve in-depth discussions of medical history, including symptoms, family history, and previous treatments.
To ensure timely treatment and adhere to documentation regulations, physicians need clear and accurate transcripts of:
- Procedure notes
- Chart notes and narratives
- General correspondence
- Independent medical evaluations
- Discharge summaries
- Consultations
- Progress reports
- History & physical
Capturing these details accurately requires careful attention to the audio recording and the ability to identify nuances in verbal dictation. The transcriptionist must also follow specific formatting and documentation standards for rheumatology notes, such as SOAP notes (Subjective, Objective, Assessment, and Plan) or other clinical documentation formats, which require consistency.
Complex Terminology: Rheumatology deals with hundreds of autoimmune diseases, inflammatory disorders, and musculoskeletal conditions. Transcriptionists working in this field must be well-versed in highly specialized terminology, medical abbreviations, and drug names, all of which can vary significantly between practitioners and institutions. Additionally, many rheumatology terms are challenging to pronounce and require careful attention to detail. Examples include complex conditions such as scleroderma, polymyositis, systemic lupus erythematosus, Wegener’s granulomatosis (now known as granulomatosis with polyangiitis), Churg-Strauss syndrome (now called eosinophilic granulomatosis with polyangiitis), mixed connective tissue disease (CTD), hyperuricemia, and Antiphospholipid Syndrome. Mastering these terms is crucial for ensuring accurate and error-free transcription in rheumatology.
Medical Jargon and Acronyms: Doctors in rheumatology use numerous acronyms, medical abbreviations, and colloquialisms that may be unfamiliar to the transcriptionist. Examples include: anticentromere antibodies – ACA; anticardiolipin antibodies – aCL; double-stranded DNA – dsDNA; psoralen ultraviolet A – PUVA, and tissue plasminogen activator – tPA. Decoding these accurately is essential to ensure the final document is correct. Additionally, rheumatologists may have varied speaking styles, accents, or speeds. This can make transcription challenging, especially when dealing with unclear or difficult-to-understand recordings.
Multiple Diagnoses: Patients with rheumatologic conditions may have multiple diagnoses, overlapping symptoms, and complex comorbidities. Examples include hypertension, cardiovascular disease, stroke, diabetes, chronic kidney disease, heart failure, lung disease, and obesity. Transcriptionists must ensure that these are captured clearly, with correct coding and terminology.
Additionally, rheumatology consultations can be lengthy, and some physicians may dictate at a fast pace, often including a lot of technical details. This can make it challenging for the transcriptionist to maintain accuracy and efficiency throughout the dictation.
Time: Turnaround time (TAT) plays a critical role in the operational efficiency of healthcare practices, directly impacting data capture and documentation. A quick and accurate TAT allows physicians to make more informed clinical decisions, ultimately enhancing patient care. Transcriptionists need to ensure precise documentation of audio recordings and meet specific TAT requirements, including STAT requests.
Improving Care with Specialized Medical Transcription Services
Enhanced Accuracy: Specialized transcription ensures precise documentation of medical records, reducing errors and improving patient outcomes.
Faster Turnaround: Professional services deliver transcriptions quickly, enabling timely access to critical patient information.
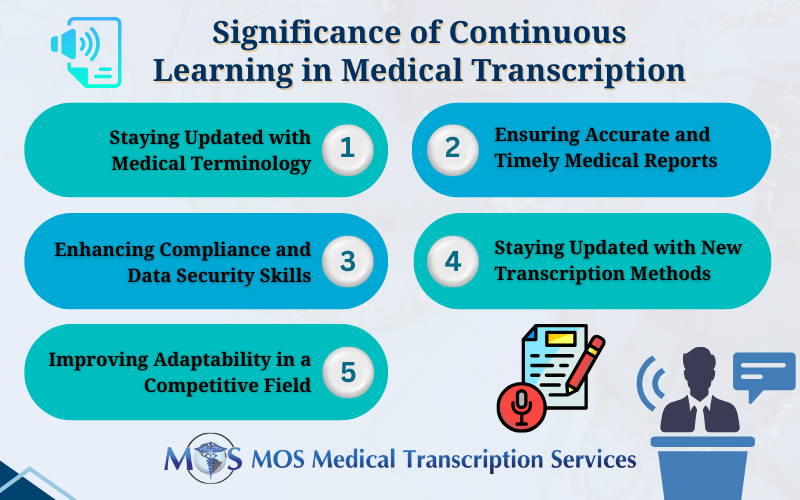
Specialized Expertise: Transcriptionists trained in the field of rheumatology can ensure correct terminology and nuanced understanding.
Improved Physician Productivity: Offloading transcription tasks frees up physicians to focus more on patient care.
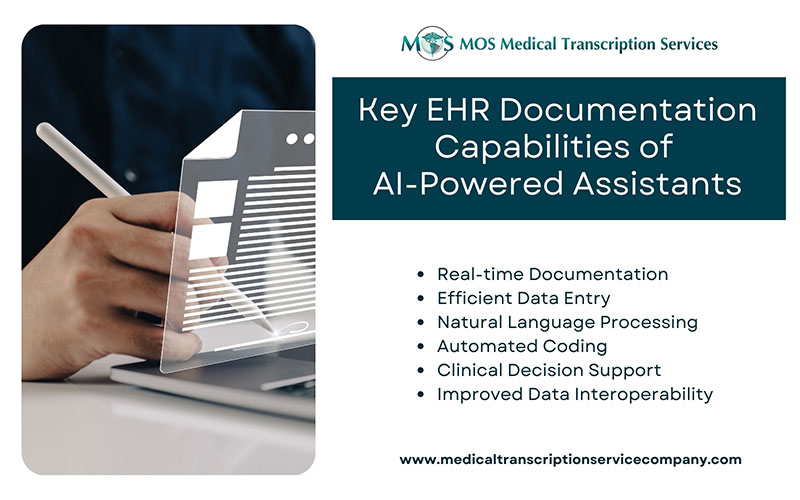
Seamless EHR Integration: Services often include compatibility with Electronic Health Record (EHR) systems for streamlined workflows.
Customized Solutions: Tailored services address specific needs of healthcare practices, enhancing operational efficiency.
One of the most significant benefits of outsourcing medical transcription is that it eliminates the need for in-house resources and reduces overhead costs. An established service provider benefits from economies of scale, handling large volumes of dictation across multiple clients. With efficient workflows, advanced technology, and a skilled workforce, these providers maintain high-quality standards while implementing robust quality control processes. They also ensure that sensitive patient information is accurately transcribed while adhering to confidentiality requirements such as HIPAA regulations.