Many physicians rely on medical transcription companies to transcribe and chart patient evaluation data in electronic health records (EHRs). EHR physician notes contain valuable medical information that is crucial to improving patient care. Medical Xpress recently reported on a new study published in the Journal of the American Medical Informatics Association which found that mining unstructured physician notes in the EHR could significantly improve diagnosis of dementia or Alzheimer’s disease (AD) for more people in hospital settings. The study was carried out by researchers from University of Wisconsin-Madison School of Nursing, William S. Middleton Memorial Veterans Hospital in Madison, and Penn State University.
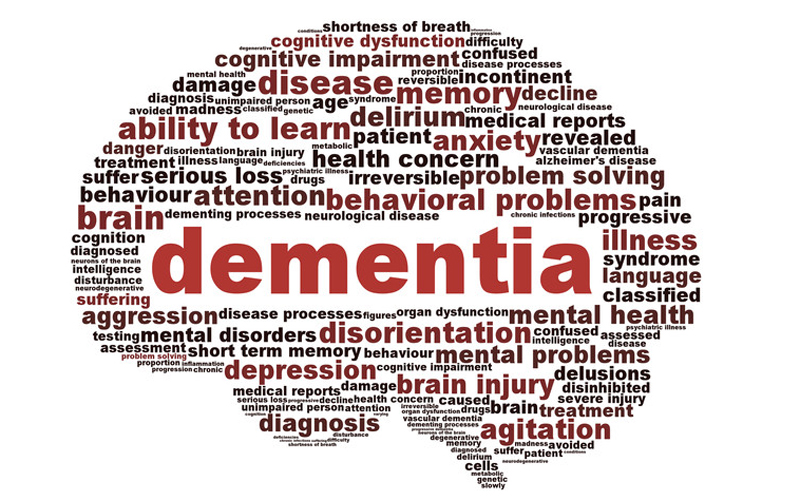
Alzheimer’s is a progressive, neurodegenerative condition and often diagnosed based on symptoms. Unlike most other medical conditions, there is no blood test or imaging test that can identify dementia with 100 percent accuracy. This complex disease is characterized by mild cognitive impairment or MCI in the primary stages. Early and repeated evaluation of cognitive change is crucial to diagnosis and treatment. Here are some facts about dementia from the World Health Organization:
- Dementia is a progressive disorder that mainly affects older people, but is not a part of aging
- This chronic condition affects memory, thinking, behavior and ability to perform daily activities
- In 2015, 50 million people lived with dementia worldwide
- A new case is diagnosed every 3 seconds
- People with dementia face discrimination
- The disease costs healthcare systems a staggering US 818 billion per year, and the predicted increase of dementia will have a huge economic impact
- Caregivers of people with dementia experience high strain
- Early diagnosis improves quality of life for people with dementia and their families
- Awareness and advocacy can improve quality of life of people with dementia and their caregivers
- More research is needed to develop new treatments and better identify causes and modifiable risk factors of dementia
If dementia is diagnosed in tests carried out in the primary care setting, patients are generally prescribed an anti-dementia medication. However, dementia goes under-recognized when people visit a hospital. According to the UW-Madison researchers, there several reasons for this:
- 40 to 60 percent of dementia cases are not been detected in the outpatient setting or even if they are, they have not been diagnosed.
- Even if the condition is identified, the primary care provider may not record dementia in the EHR to save patients from the stigma associated with the condition.
- Racial and ethnic minorities or people from low socio-economic background are at highest risk for developing dementia, but they tend to have less access to the primary care or specialized memory care clinics where AD is initially diagnosed.
When these people visit the hospital for the treatment of a chronic condition, the memory and reasoning problems associated with AD and other kinds of dementia go under-recognized.
In the hospital and recovery clinic, physicians and nurses record their observations and interactions with a patient, the treatment plan, and how the patient responded in the electronic health record. The UW-Madison study found that these EHR ‘progress notes’ or ‘provider notes’ could provide vital clues about the patient’s cognitive function.
The researchers reviewed the notes from unstructured fields in the EHRs of 343 people diagnosed with dementia to identify words and phrases that describe cognitive dysfunction such as “forgetful at times, “increased confusion in the evening,” “disoriented and agitated,” “limited by confusion” and “finding it hard to find words”. They found that 90% of the EHRs had notes signifying one or more of these descriptors of confusion or cognition.
Medical Xpress recently reported on another new study which found that hospitals in the UK recognized dementia in under two-thirds of people after they have been admitted for a different reason. Hospitals tend to miss dementia regardless of prior diagnosis, according to this UCL-led study. Similar to the UW-Madison study, the researchers found that it is those of ethnic minority backgrounds that are almost twice as likely to have missed diagnoses in general hospitals compared to white patients. The researchers also reported that hospitals are also less likely to identify dementia for single people, younger people, and people with more severe physical illness.
The UW-Madison team suggests that clinicians flag the common terms that describe cognitive dysfunction as they record their notes. This will improve care in many ways:
- Flagging their notes will allow physicians and nurses and future care providers to make customized prescription and treatment decisions targeting their patients’ cognitive functioning.
- It may also help them refer more unrecognized dementia cases to follow-up care and subsequent diagnosis
- Flagging EHR notes may improve diagnosis and treatment rates for people from the racial and economic groups who are more likely to go directly to a hospital clinic or emergency room for medical care
- Highlighting progress notes with dementia-related terms could prove very useful for research into the causes and treatment of dementia
Reports say that up to 80% of all health record data is trapped in this unstructured text, which includes lab reports, pharmacy systems, discharge summaries, scanned documents, e-faxes, and e-mail messages. Medical transcription outsourcing helps healthcare providers ensure neat, legible, type-written notes within electronic health records (EHRs). Many health systems are now looking to natural language processing (NLP) tools to mine and analyze these free-text notes and understand what going on with their patients.