Table of Contents
Electronic medical records (EMRs) act as a centralized repository for patient information, including clinical notes, treatment plans, medication records, and billing details. In all specialties, EMR documentation accuracy is essential for delivering personalized care and monitoring patient progress over time. Medical transcription services and standardized workflows play a key role in reducing electronic medical record errors caused by incomplete or inconsistent documentation.
EMRs are designed to improve the efficiency, accessibility, and organization of patient information. However, errors can occur. The golden rule for healthcare providers is: if it’s not documented, it didn’t happen. Avoiding medical record errors starts with accurate, timely medical record documentation supported by reliable medical transcription services. Skilled medical transcriptionists can ensure accurate and timely documentation of medical history, diagnoses, and treatment in the EMR, so that physicians have the information they need to diagnose and treat the patient. Taking steps to minimize the likelihood of errors in EMRs is essential for upholding patient safety and delivering high-quality healthcare.
Common Electronic Medical Record Errors
Here are some common errors in EMRs (Electronic Medical Records) that can impact patient care:
- Data Entry Errors: This includes typos, misspellings, or incorrect information entered into fields, improper data formats, and duplicate records or inaccurate patient details.
- Incorrect Patient Information: Incorrect patient identifiers, mixed-up records, or outdated details can result in significant medical risks and errors.
- Incomplete Documentation: Missing vital clinical notes, treatment plans, or test results and failure to document patient interactions or follow-up care increase the likelihood of clinical documentation errors.
- Copy-Paste Practices: This refers to overuse of copied text from previous notes, causing outdated or irrelevant information to persist. It also includes lab results, prescriptions, or referrals filed under the wrong patient or category.
- Interface Errors: Problems can occur with data synchronization between EMR systems and lab or imaging systems.
- Lack of Standardization: Use of non-standardized templates can make records inconsistent or hard to interpret.
- Security and Access Issues: Unauthorized access or failure to restrict sensitive data to relevant users, and insufficient encryption increase the risk of breaches.
- Overreliance on Automation: This can lead to errors in automated alerts, medication interactions, or clinical decision support tools.
- Outdated or Non-compliant Records: This results from failing to update records promptly or maintain HIPAA-compliant documentation practices.
Identifying and addressing these issues is critical to ensuring EMRs effectively support patient care and operational efficiency.
The Hidden Costs of EHR Documentation Errors in Healthcare
Here’s what makes EHR documentation errors a costly challenge:
- Causes Physician Burnout and impacts Data Quality
EHR data entry takes up physicians’ valuable time. According to research published by JAMA Network in 2023, providers may be spending more time interacting with EHRs than with their patients. On average, they spend over 36 minutes working in the EHR for every 30-minute patient encounter, highlighting the growing administrative burden placed on clinicians.
Physician burnout is strongly linked to an increase in documentation errors, which can negatively impact patient safety and outcomes. Burnout can lead to cognitive fatigue, making it harder for physicians to focus on complex tasks like accurate documentation, according to research from the National Institutes of Health (NIH).
- Compromises Patient Safety
EHR data entry errors can significantly compromise patient safety. These errors, whether due to manual entry mistakes, system design flaws, or information overload, can lead to inaccurate patient information and ID errors, misdiagnoses, incorrect treatments, and medication errors, and ultimately, patient harm.
- Claim Denials and Audits
Typos or inaccurate data entry in critical fields within the EHR system can directly lead to claim denials and audits, impacting revenue cycle management and potentially lead to penalties. Incomplete, inaccurate, or outdated documentation can cause claims to be rejected or denied by payers, necessitating time-consuming corrections and appeals.
- Increases Malpractice Risks
A wide-ranging 2020 report, Malpractice Claims Report titled “EHR Documentation Errors Still Far Too Common” analyzed data from nearly 12,000 events pertaining to more than 20,000 closed claims across a 10-year period from 2010 to 2019. The study found that average indemnity paid for physicians’ medical malpractice claims increased 20 percent during the study period, to $411,053. According to the study, documentation accounts for the majority of EHR-related risk issues, representing 72% of reported cases. The researchers noted that the risks typically occur when users:
- select the wrong dropdown
- view the wrong screen
- enter outdated information, or
- mistakenly document in the wrong patient’s chart
Other common sources of risk include system-related problems such as poor interface design, indiscriminate use of the copy-paste function, errors introduced during system conversions, lack of EHR training and education, health records in multiple formats and stored in several locations, and overall challenges with EHR usability.
10 Best Practices for Reducing EMR Documentation Errors
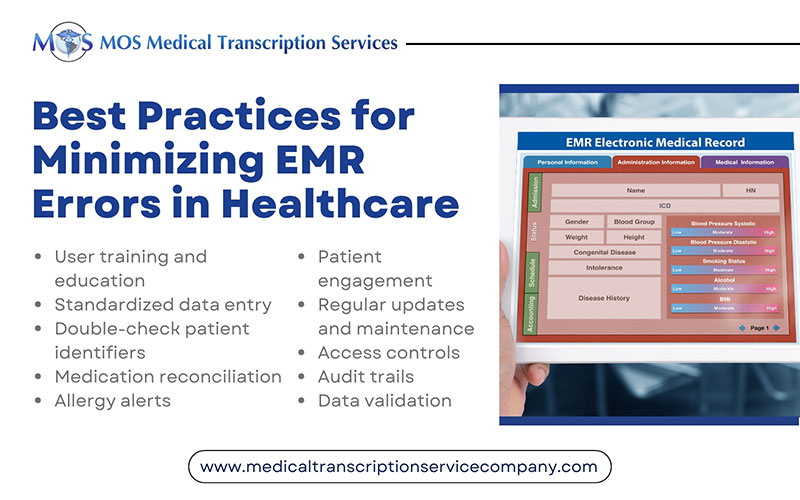
Here are some tips to prevent electronic medical record errors and help healthcare providers and institutions minimize the likelihood of errors in EMRs:
- User training and education: Ensure that all healthcare professionals who use the EMR system are adequately trained on its features and functions. Provide ongoing training and updates to keep users informed about any system changes or enhancements.
- Standardized data entry: Establish standardized protocols and templates for data entry to ensure consistency and accuracy. Use drop-down menus, checkboxes, and predefined options wherever possible to reduce free-text entry errors.
- Double-check patient identifiers: Verify patient identities using multiple identifiers (e.g., name, date of birth, medical record number) to prevent mix-ups and duplicate records.
- Medication reconciliation: Implement a robust medication reconciliation process to ensure that medications are accurately recorded.
- Allergy alerts: Configure the EMR to issue allergy alerts and warnings when prescribing medications or treatments that patients are known to be allergic to.
- Patient engagement: Encourage patients to review their electronic records for accuracy and report any discrepancies or errors promptly.
- Regular updates and maintenance: Keep the EMR system up-to-date with the latest software updates, patches, and security enhancements to prevent system vulnerabilities that could lead to errors.
- Access controls: Implement strict access controls and user permissions to ensure that only authorized personnel can access and modify patient records.
- Audit trails: Enable audit trails within the EMR system to track changes made to patient records, allowing for accountability and transparency.
- Data validation: Use data validation rules and algorithms to flag or prevent erroneous entries, such as illogical vital sign values or abnormal laboratory results.
Expanding Role of Generative AI in Clinical Documentation
Generative AI is rapidly advancing to help close documentation gaps in EHR systems. Driven by the rise of chatbot interfaces like ChatGPT, health IT vendors and healthcare systems are increasingly piloting generative AI tools to streamline clinical documentation. According to a recent HLTH report, healthcare AI startup WorkDone has developed an AI-powered compliance co-pilot that integrates directly with hospital EHRs using standards like HL7, FHIR, and other industry protocols. This tool monitors clinical workflows in real time to identify and address issues such as missing discharge summaries or incorrect medication timing.
However, while these technologies show promise in reducing the documentation burden linked to clinician burnout and providing accurate medical records.
Tech Target reported on a study of 10,000 physicians and staff at The Permanente Medical Group that assessed the adoption of ambient AI scribes. Physicians reported that ambient AI improved the quality of patient conversations. Providers experienced reduced after-hours EHR documentation workload.
However, providers must review all AI-generated documentation drafts to ensure accuracy and maintain patient safety. The report noted that a 2023 study found that ambient AI struggles to capture non-lexical conversational sounds (NLCSes), such as “mm-hm” or “uh-uh,” which often carry clinical significance.
Critical error rates were:
- Overall word error rate: ~12%.
- NLCS word error rate: 40%–57%.
- For clinically meaningful NLCSes, the error rate soared to 94.7%–98.7%.
“Implementation will require improvements in accuracy, completeness and safety,” the authors wrote. “Given the safety concerns, initial implementation will require physician review.”(TechTarget).
How Medical Transcription Services Reduce EMR Errors
Medical transcription services help reduce EMR errors by converting clinician dictation into accurate, structured, and standardized medical records. Trained medical transcriptionists, supported by advanced speech recognition technology, ensure that diagnoses, procedures, medications, and clinical observations are captured clearly and completely. Built-in quality checks identify missing information, inconsistencies, and terminology errors before records are finalized, minimizing documentation gaps caused by rushed note entry or manual typing. By delivering precise, timely, and compliant documentation, an experienced medical transcription company improves record integrity, supports better clinical decision-making, and enhances patient safety.