Table of Contents
Operative report transcription plays a critical role in healthcare reimbursement. Inaccurate or delayed operative notes are one of the leading causes of claim denials, reimbursement delays, and revenue loss for medical practices. When surgical documentation is incomplete, even properly performed procedures can go unpaid.
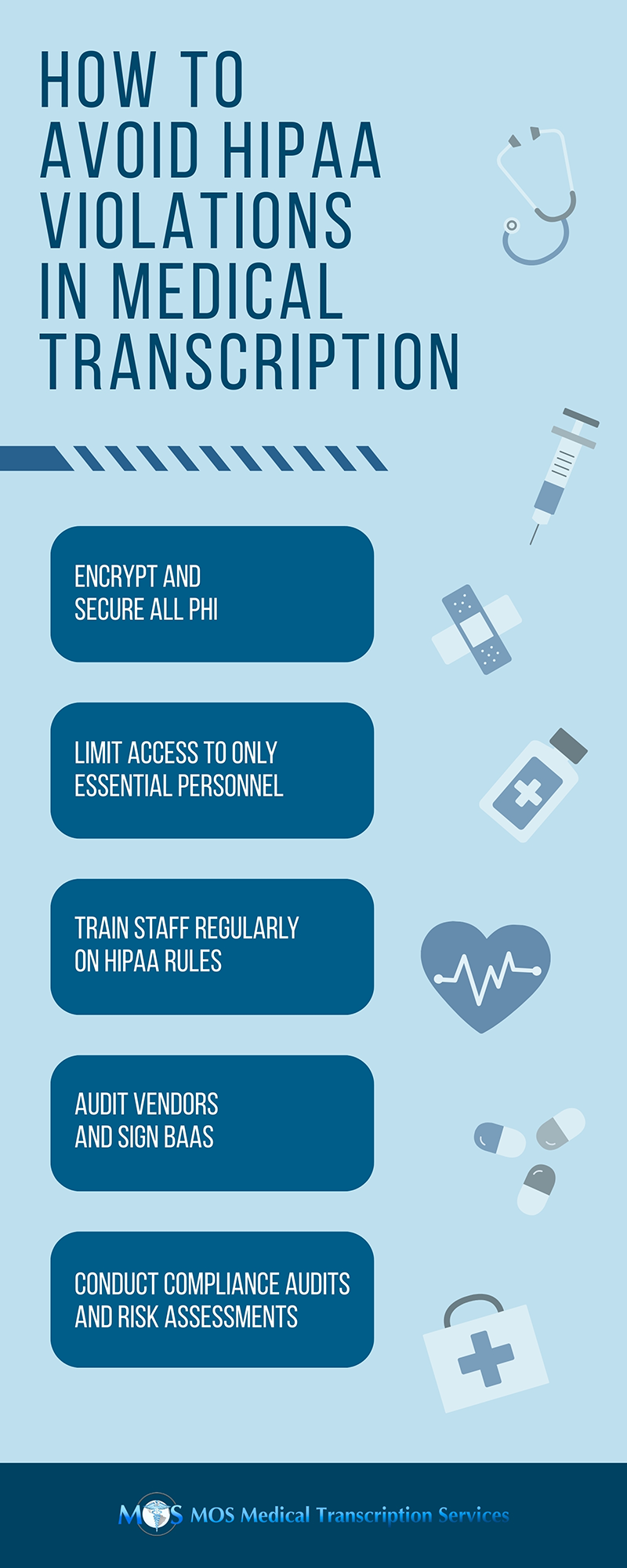
If your practice is experiencing reimbursement delays, the problem may not be your billing team — it may be your surgical documentation workflow. With increasing pressure on healthcare providers, timely and precise HIPAA compliant medical transcription services have become essential for smooth claims processing and stable revenue cycle management.
Why Operative Documentation Affects Reimbursement
Operative notes are important in the claims process, documenting the patient’s preoperative diagnosis, reasons for the procedure, and final surgical outcomes. These details determine how a case is coded, billed, and reviewed for compliance. Insurance companies rely on these reports to ensure accurate coding, medical necessity, and appropriate reimbursement rates.
Inaccurate or incomplete reports make it difficult for insurers to assess the full scope of care provided, resulting in claim rejections or payment delays. Missing secondary procedures or misidentified codes can trigger denials that require additional administrative work and resubmission.
Common Operative Report Transcription Errors That Cause Claim Denials
Surgical documentation presents several challenges that can delay reimbursement. The most common include:
- Inaccurate Reporting
Even minor errors in procedure descriptions can significantly impact surgical claim processing. Misidentified techniques or incorrectly noted procedural steps can prevent insurers from validating services rendered, resulting in delays or denials.
- Inconsistent Terminology
Consistency in medical terminology is essential for clarity. Variations in abbreviations or anatomical terms can confuse payers during claim review. Consistent and standardized language reduces discrepancies between what was performed and what is reflected in the report, supporting timely reimbursement.
- Missing Clinical Information
Small but critical details such as the patient’s medical history or specific post-operative instructions can easily be overlooked during documentation. Omitting these can create documentation gaps in operative notes, leading to requests for additional information, claim resubmissions, and delayed healthcare reimbursement approvals.
- Poor Dictation Quality
The quality of the dictation is a key factor in transcription accuracy. Heavy accents, unclear speech, rushed dictation, fragmented phrasing, and incomplete sentences can result in documentation errors. These issues make it difficult for transcriptionists to capture the full scope of the procedure accurately, affecting coding accuracy, claim denials, and reimbursement timelines.
- Ineffective EHR Integration
Effective transcription requires seamless access to patient data, prior imaging studies, and medical histories. When EHR systems are not properly connected with transcription tools, transcriptionists may lack necessary clinical context. This can result in incomplete surgical reports and reimbursement delays.
Surgical documentation provides a detailed record of a surgical procedure, capturing essential information that drives the claims and reimbursement process. Understanding the key sections of an operative note is crucial for identifying potential transcription errors that may lead to claim delays or denials.
- Preoperative Diagnosis
This section outlines the patient’s condition prior to surgery, detailing the diagnosis that led to the need for the procedure. An accurate preoperative diagnosis ensures that the services are medically necessary and supports the case for insurance reimbursement.
- Indications for Surgery
The indications section explains why the surgery was performed, including the patient’s medical history, previous treatments, and any other factors that led to the decision to proceed with surgery. This section must clearly justify the procedure to meet payer requirements for medical necessity.
- Description of the Procedure
This is the most detailed part of the operative note, describing the surgical steps taken during the procedure. It must include information such as the techniques used, the findings during surgery, and any complications that arose. Accurate documentation here is essential for proper coding and to avoid claim rejections due to ambiguity.
- Findings
This records the surgeon’s observations during the procedure. Any unexpected findings, complications, or alterations in the planned procedure should be documented thoroughly. Inaccuracies in this section can lead to issues with both medical necessity and procedure coding.
- Postoperative Diagnosis
The postoperative diagnosis section provides a summary of the patient’s condition after surgery, including any new findings or complications. It mirrors the preoperative diagnosis but can include additional insights, especially if the surgery revealed new information. This ensures that the post-surgery care plan aligns with the procedure performed.
- Follow-up Care
Follow-up care outlines the next steps in the patient’s care, including any follow-up treatments, medications, or recommendations. It provides essential information for insurance companies to understand the full scope of care required after surgery and further supports claims for reimbursement.
How Reimbursement Delays Impact Practices
Delayed or inaccurate operative reports can affect a practice’s entire function, from cash flow to operational efficiency:
- Cash Flow Disruptions: Delays in reimbursement can create immediate cash flow problems. Practices rely on steady payments to cover daily expenses, from staff salaries to equipment costs. When those payments are delayed, it forces providers to make difficult financial decisions.
- Administrative Burden: Denied or delayed claims lead to additional administrative work. Staff must spend time appealing denials, resubmitting reports, and responding to insurer follow-ups. This reduces the time spent on patient care and increases overhead costs.
- Operational Strain: Extended delays can stretch a practice’s resources thin. If reimbursements don’t arrive as expected, providers may face difficulties managing operating costs, staff wages, and other financial obligations. In the long term, these challenges can lead to a strained workforce and hinder practice growth.
- Financial Instability: Ultimately, persistent delays and denials can lead to financial instability for the practice. Without predictable, timely payments, healthcare providers may find it difficult to manage cash flow, invest in new equipment, or retain staff. This can affect the quality of care and may even lead to higher turnover rates.
How AI-powered Tools Improve Medical Transcription
AI-powered tools are transforming how operative reports are transcribed, making the process faster, more accurate, and efficient. By leveraging advanced algorithms, these tools streamline the transcription process, reducing human errors and improving the quality of the final report.
- Increased Accuracy: AI tools minimize transcription errors by accurately capturing complex medical terminology and procedure codes.
- Faster Turnaround: Real-time processing speeds up the transcription, ensuring quicker availability of reports for claims submission.
- Consistency: AI ensures standardization across all reports, reducing inconsistencies caused by different dictation styles.
- System Integration: Seamless integration with EHR and other systems streamlines clinical data entry and reduces manual work.
Practices can rely on medical transcription services that incorporate AI-powered tools to significantly enhance their documentation processes. These agencies not only improve the accuracy and speed of operative report transcription but also ensure compliance with coding standards. By partnering with an experienced service provider, practices can streamline surgical documentation workflows, supporting faster claim processing and smoother reimbursement cycles.