Table of Contents
A physician’s office visit, also referred to as a consultation, is a meeting between a patient and a healthcare professional to address health concerns, receive preventive care, or manage chronic conditions. The typical components of an office visit are review of medical history and current symptoms, a physical exam, diagnostic testing (if needed), discussion of findings and treatment options, and patient education and counseling. All of this information needs to be documented in the electronic health record (EHR). Outsourcing medical transcription is a practical option for providers to manage outpatient documentation, focus on care, and ensure accurate clinical summaries of office visits. By reducing the physician documentation burden, it allows them focus on the patient and clinical activities rather than EHR data entry during the encounter.
Significance of Clinical Summaries of Office Visits
Office visits are critical for maintaining continuity of care and ensuring patients stay on track with their health goals. A clinical summary is a document provided to patients after an office visit that highlights key details of the encounter. It ensures that patients clearly understand their diagnosis, treatment plan, and follow-up instructions, while also supporting continuity of care across providers. The goals of the patient encounter summary are to:
- Improve patient and family engagement by giving patients a written record of their visit. Providing patients and their families with access to EHR information helps engage them in healthy behaviors, self-managing chronic conditions, and improving care quality by identifying and correcting data errors.
- Enhance communication between patients and healthcare providers.
- Support collaboration among multiple care providers.
- Meet regulatory requirements, such as those under the HITECH Act and Meaningful Use.
However, while ensuring a timely and accurate clinical summary after each office visit is important for these reasons, there are certain challenges involved in meeting this goal. Poor documentation practices lead to incomplete and inaccurate records, affecting patient management, continuity of patient care, and medicolegal issues, according to research published in BMJ Health Care Informatics in 2023.
Key Challenges in Generating Clinical Summaries
There are several challenges in generating clinical summaries:
- Time Spent on Documentation: A 2024 survey by the American Medical Informatics Association (AMIA) revealed that 77.42% of healthcare professionals reported finishing work later than desired or needing to work at home due to excessive documentation tasks.
- Impact on Patient Care: The time or effort required for clinical note-taking hampers patient care.
- Difficulty to Navigate for Patients: EHR-generated after-visit summaries (AVS) may be difficult for patients to understand due to lack of key content, poor formatting, and technical jargon.
- Challenges with AI-Generated Summaries: Hospitals report difficulties in validating AI-generated EHR documentation quality and clinical summaries, with concerns about the accuracy and reliability of these automated tools, according to a STAT10 report.
Poorly crafted summaries and progress notes can have several implications for healthcare practices. The substantial time spent on documentation affects focus on patient care, also leading to clinician burnout and decreased job satisfaction. Inadequate or unclear clinical summaries can negatively impact patient understanding and engagement, impact overall satisfaction with care. Incomplete or inaccurate documentation can lead to medicolegal issues, including increased odds of cases closing with indemnity payments.
For improving patient care with clinical visit summaries, providers should ensure they contain relevant content. EHRs should be organized to ensure that they create content that supports patient self-management. Patients can be given print material that is easy-to-understand.
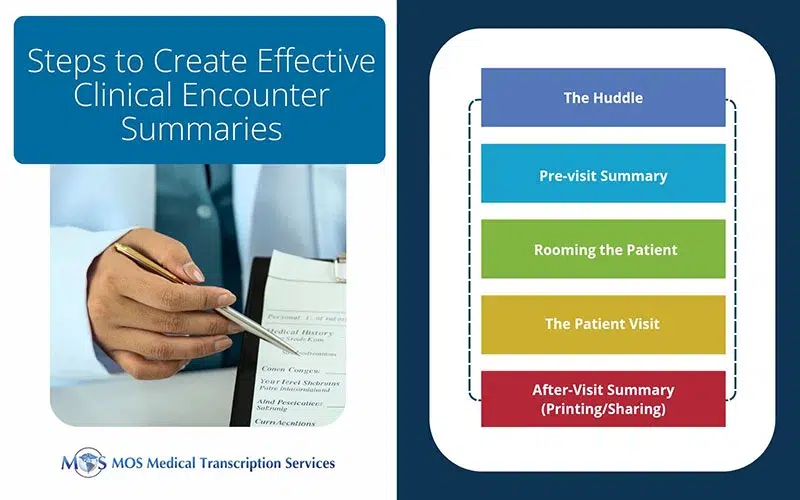
Five Steps to Create Effective Clinical Encounter Summaries
HealthIT.gov has identified 5 key practice workflow steps to provide patients with an accurate clinical summary at the end of an office visit:
- The Huddle: This is a brief meeting of the care team including the physician to prepare for each patient and improve the team’s decision-making efficiency at the time the patient is in the office.
- The Pre-visit Summary: This is a printed document that is given to the patient in the waiting room by the front desk staff. It should include key information such as medication list, allergy list, health maintenance items, tobacco use status, problem list, and evidence-based monitoring for certain chronic illnesses. The patient should be instructed to review the list before seeing the care team so that changes can be made if needed.
- Rooming the Patient: This step involves the clinical assistant checking vital signs and reviewing the pre-visit summary with the patient and updating the EHR with any changes.
- The Patient Visit: The provider makes clinical decisions in collaboration with the patient on tests, treatments and referrals and enters these as orders in the EHR.
- Printing the After-Visit Summary: At the end of the visit the provider reviews the clinical summary and provides the patient with a copy. The summary can also be delivered through the EHR patient portal, or secure e-mail.
While following these basic steps, providers can improve medical record accuracy and the clinical summary in various ways:
- Highlight important clinical information with bold formatting
- Highlight health reminders, referrals, procedures, medications, and other important categories of information
- Ensure that their facility’s phone number and other contact information is clearly displayed
- Use plain language and explain complex terms which some patients may find it difficult to understand
- Avoid a lengthy summary
- Involve patients in creating the summary in order to include the information they would find useful
- Customize the content to meet patient needs and ask for feedback
Solutions to Improve Clinical Summary Generation
Outsourcing Medical Transcription
Medical transcription services have professionals who are trained to create precise, structured clinical summaries from physician notes or voice recordings, reducing errors in patient records. Physicians save significant time on writing summaries and focus on patient care. Outsourced transcription services follow templates and EHR-compatible formats, ensuring uniform summaries across patients and visits. Reliable vendors maintain strict data security protocols, protecting sensitive patient information.
EHR Integration & AI Assistance
Many transcription services integrate directly with EHR systems, automatically uploading summaries and supporting structured documentation. AI-assisted transcription can pre-fill certain fields, while human transcriptionists review for accuracy, combining speed and precision.
Effective Template Use
Transcriptionists can adapt templates for different specialties to capture relevant details efficiently. Using standardized templates and clear guidelines improves the clarity and completeness of clinical summaries.
Working with an experienced medical transcription company enables healthcare providers to implement best practices for generating office visit summaries. Ensuring high quality, accurate, and timely outpatient documentation improves patient care, compliance, and workflow efficiency, while reducing physician burnout.