Table of Contents
In the fast-paced digital healthcare scenario, accurate and timely clinical documentation is essential for delivering high-quality patient care. One proven method to improve documentation efficiency is through the use of SOAP notes (Subjective, Objective, Assessment, Plan)—a structured format that helps clinicians clearly document patient encounters, treatment plans, and medical progress. By enhancing clinical workflow and communication, SOAP notes support better care coordination and compliance with healthcare standards. However, given the time-intensive nature of documentation, many healthcare providers turn to medical transcription outsourcing services. Outsourcing SOAP note transcription ensures fast, accurate clinical documentation, allowing physicians to maintain high standards of record-keeping while devoting more time to focus on what really matters-patient care.
Understanding the Structure of SOAP Notes
SOAP notes are a widely used tool for medical charting. Understanding their structure is essential for creating accurate, effective, and comprehensive electronic health records (EHRs). While healthcare professionals aren’t legally required to use SOAP documents, they are mandated by law to maintain detailed and accurate medical records for purposes such as billing and patient safety.
SOAP notes aren’t the only format for documentation, they are widely preferred by healthcare providers due to their standardized and consistent structure. Enhancing medical records with the SOAP note format facilitates continuity of care, streamlined communication, and enhanced patient outcomes.
Let’s explore the four separate sections in this format:
- 1. Subjective: The Patient’s Perspective
The subjective section documents the patient’s personal experience and insights into their condition. This typically includes their symptoms, concerns, medical history, and any other information shared during the consultation. Accurate documentation of this section is crucial, as it directly influences further examination and treatment.
- 2. Objective: The Clinician’s Observations
The objective section records measurable, observable, and testable data collected by healthcare professionals. This may include vital signs (such as blood pressure or heart rate), physical examination findings, lab results, and any relevant diagnostic tests. It’s important that this section remains free of personal interpretation to ensure an accurate clinical assessment, diagnosis, and treatment.
- 3. Assessment: The Provider’s Interpretation
The assessment section is a critical part of SOAP documentation, as it reflects the healthcare provider’s clinical judgment about the patient’s condition. Here, the clinician synthesizes the subjective and objective data to provide a primary diagnosis or list of potential diagnoses. This section is essential for informed decision-making, allowing healthcare providers to determine the next steps in treatment.
- 4. Plan: The Final Step
Finally, the plan section outlines the proposed course of action. It includes recommendations for further testing, medications, treatments, referrals, or lifestyle changes. Functioning as a roadmap for ongoing care, this section ensures that both the patient and healthcare team are aligned in their approach to treatment.
Key Benefits of Integrating SOAP Notes in Your Practice
Clear, organized, and efficient documentation is essential in the fast-paced healthcare environment to improve efficiency, quality, and ensure compliance. Serving as a framework for documenting patient encounters, SOAP notes streamline the process of diagnosis, treatment, and ongoing care. Integrating structured medical notes into your practice unlock a range of benefits such as streamlined processes, improved communication, and enhanced patient outcomes. Let’s explore it in detail:
- 1. Improved Organization and Communication
SOAP documents help healthcare providers to structure patient information in a consistent and logical manner. Breaking the documentation into four distinct sections makes it easier to track the progression of the patient’s condition, treatment, and response. This facilitates seamless communication between healthcare providers, ensuring no critical details are overlooked. Using SOAP notes to streamline clinical workflows reduces miscommunication, enhances collaboration, and ensures continuity of care.
- 2. Streamlined Billing and Insurance Process
Medical records not only create and share patient data, but also serve to justify the services rendered to insurance companies. Clinical documents form the foundation for coding and billing processes, where medical coders and billers translate clinical procedures into standardized codes for payment. SOAP documents provide clinical evidence of the patient’s condition and the necessity for specific treatments or procedures, playing a crucial role in supporting accurate billing. These notes ensure that the billing reflects the actual care provided, minimizing the chances of claim rejections and helping to streamline the insurance reimbursement process.
- 3. Integration with Healthcare IT Infrastructure
Electronic SOAP templates can be integrated into digital systems such as Electronic Health Records (EHRs) or Practice Management Software (PMS). These systems allow for easy retrieval, sharing, and updating of patient records, ensuring that providers work with the most current information. Real-time accessibility reduces manual errors and optimizes workflows in healthcare organizations.
- 4. Facilitates Timely Decision-Making
With SOAP documents, healthcare providers have quick access to accurate case details, enabling faster decision-making. The structured format highlights key information such as symptoms, clinical findings, and ongoing treatment plans, reducing the risk of mistakes or omissions during care. This is especially beneficial in urgent or complex situations, where timely and well-informed decisions can significantly impact health outcomes.
Best Practices to Implement EMR SOAP integration
Implementing SOAP documentation into your healthcare organization requires a strategic approach based on your specific needs and requirements. Here are some best practices for effective SOAP note writing:
- Standardize the Format: Standardizing the format ensures that every staff member follows the same structure, enhancing consistency across your practice. Whether for solo practitioners or larger teams, using a uniform template improves communication and streamlines collaboration.
- Ensure a Comprehensive Subjective Section: In the subjective section, it’s crucial to document the patient’s symptoms and concerns in detail. A complete and accurate description—such as the duration, intensity, and triggers of pain—helps healthcare providers better understand the causes and guide the treatment process.
- Accurately Record the Objective Section: The objective section must be documented accurately, with correct units and reference ranges for vital signs, lab results, and clinical examination findings. This ensures that only precise, measurable data is recorded, providing a complete picture of the patient’s health status for further assessment.
- Provide a Clear and Concise Assessment: The assessment section should summarize your clinical impression based on both subjective and objective data. Avoid vague language and be specific about the diagnosis, differential diagnoses, or the severity of the condition.
- Develop an Actionable Plan: The plan section should outline actionable steps, such as treatment recommendations, diagnostic tests, follow-up visits, or referrals to specialists. It should provide a well-structured, detailed strategy for holistic and coordinated care, ensuring successful health outcomes.
- Review and Update Notes Regularly: SOAP notes are not just patient records; they are an effective communication tool that needs regular updates. Keeping records current helps monitor the patient’s progress, ensures continuity of care, and improves the accuracy of medical claims.
- Train Employees: Provide ongoing SOAP format documentation training to ensure proficiency in using the format consistently and effectively. Encourage team members to periodically review and discuss SOAP notes to identify areas for improvement and maintain high standards.
Following these best practices ensures smooth SOAP note integration, improving documentation, patient care, and team communication.
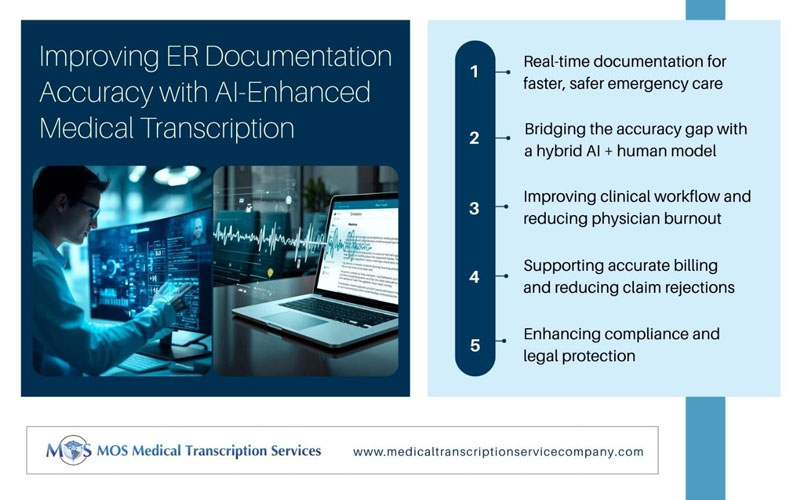
Enhance SOAP Documentation with Medical Transcription Outsourcing
Outsourcing transcription for SOAP notes offers a strategic edge by boosting both clinical documentation accuracy and operational efficiency. With experienced medical transcriptionists converting voice recordings into structured SOAP note format in real-time, practices can maintain up-to-date, error-free patient records without shifting focus away from patient care. This approach streamlines workflow, enhances clinical decision-making, and reduces documentation delays. By ensuring accurate, consistent, and timely SOAP note documentation, medical transcription services support better patient outcomes and improve overall healthcare practice management. In a healthcare landscape where efficiency and precision are critical, outsourcing has become a smart solution for maintaining high standards in medical recordkeeping.