Charting is a necessary element of nurses’ daily tasks. In addition to charting, nurses have numerous roles and responsibilities and outsourcing medical transcription is a practical strategy to maintain error-free EHR documentation. According to the American Nurses Association (ANA), clear and accurate documentation is essential for safe, quality, evidence-based nursing practice. Proper charting prevents errors, supports accurate assessment and diagnosis, and improves patient outcomes.
Table of Contents

When it comes to nursing documentation, knowing how to accurately document a patient in the EHR is critical, meaning the nurses should be EHR-savvy. They should be well aware of the risks of erroneous and incomplete documentation. Improper documentation can lead to legal issues. An article published in American Nurse noted that nursing documentation with incorrect patient information is responsible for up to 72% of all electronic health record (EHR) related risk issues.
What are the Features of Good Quality Nursing Documentation?
Documentation of nurses’ work is critical as well for effective communication with the healthcare team. According to the ANA, high quality nursing documentation is that which is:
- Accessible
- Timely
- Contemporaneous
- Concise
- Thorough
- Organized
- Confidential
- Reflective of the nursing process
- Legible/readable (particularly in terms of the resolution and related qualities of EHR content as it is displayed on the screens of various devices)
- Retrievable on a permanent basis in a nursing-specific manner
Good documentation provides a chronological record of the patient’s progress, the care provided, and how the patient responded to that care, noted Cherlyn Shultz-Ruth, Dean of Nursing at Arizona College of Nursing — Dallas Campus in an article on the Importance Of Quality Charting In Nursing published by the Arizona College of Nursing.
Legal Significance of Nursing Documentation
Nursing records have immense legal significance. Meticulous charting plays a vital role in ensuring both patient well-being and professional integrity. Experts highlight that by maintaining effective documentation, nurses not only safeguard patients and improve care outcomes, but also protect themselves.
Nurses’ record-keeping practices are under increasing scrutiny. Nurses should stay up to date with the legal requirements and best practices in record-keeping. They should ensure that the health care record provides an accurate account of treatment, care planning and delivery states a Nursing Times article. In the event of malpractice litigation, providers need to present evidence of proper charting and documentation to show that standards of care were maintained. From the legal perspective, Nursing Times states that the documentation should demonstrate:
- The nurse’s assessment and the patient care planned and provided
- Pertinent information about the patient’s condition at any point
- Measures taken by the nurse to meet the patient’s needs
- Evidence that the nurse has taken all appropriate steps to care for the patient and that patient safety has not been compromised by any action or omission
- Documentation of arrangements made by the nurse for the continuing care of the patient
Nursing records that are incomplete, inaccurate, untimely, illegible or inaccessible, or that are false or ambiguous can obstruct legal fact finding, endanger the legal rights, claims, and defense of both patients and health care providers, and increase risk of liability of the healthcare organization and providers.
Medical Records – Common Mistakes to Avoid
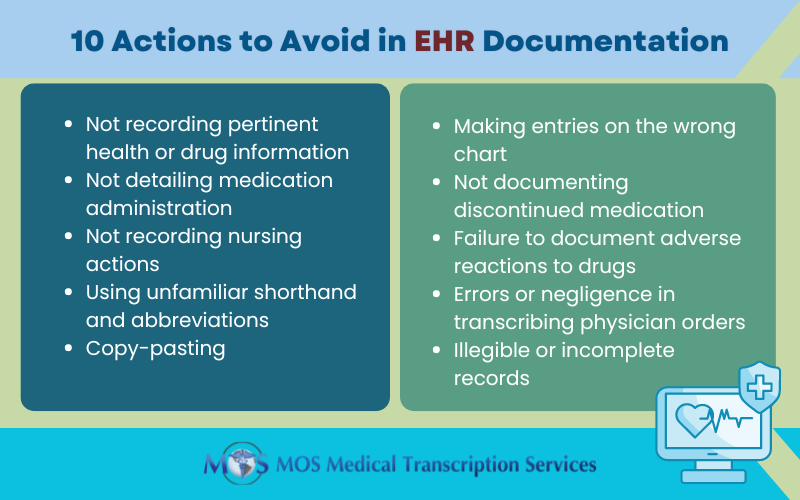
Here are 10 actions to avoid during EHR documentation
- 1. Not recording pertinent health or drug information: Effective charting means avoiding fragmented documentation and providing information necessary for the continuity of care. It’s necessary to document food and drug allergies, diseases, or chronic health problems. Nurses should record such information in their notes and on the admission sheet, and alert other staff members to do so. Not doing so could result in the nurse being accused of negligence.
- 2. Not detailing medication administration: Nurses should record the dose, route, and time of every medication given to the patient. They should ensure that only medications that are prescribed are administered and investigate if they suspect that medication may have been given but not recorded.
- 3. Not recording nursing actions: To ensure timely recording of all care provided, experts recommend inserting flow sheets in the patient’s chart for review at the end of each shift. This will provide a starting point for each staff member at the start of and through the shift.
- 4. Using unfamiliar shorthand and abbreviations: As far as possible, nurses should avoid using unfamiliar shorthand and abbreviations and don’t clearly convey the patient’s condition.
- 5. Copy-pasting: Nurses should avoid copy-pasting from other team members. Make your own assessment of the patient and document it.
- 6. Making entries on the wrong chart: Recording on the wrong chart can occur, for example, if two patients have same last name, share same room, suffer the same condition, or see the same doctor. This error can become part of a permanent record, resulting negligence and medical malpractice. Best practice is to highlight patients’ names on charts and medication records and check their identity before administering medications.
- 7. Not documenting discontinued medication: If the physician discontinued a medication and the nurse did not document this, the patient may continue receiving the drug – with disastrous medical consequences. The nurses can be sued for negligence. To avoid this, the nurse should crosscheck the physician’s orders and medication sheet before giving any medication.
- 8. Failure to document adverse reactions to drugs: Nurses should be vigilant for adverse effects in patients. Certain drugs can lead to harmful reactions in some patients. Nurses should document such adverse reactions and follow them with the physician.
- 9. Errors or negligence in transcribing physician orders: Nurses receive physician orders face-to-face, and via telephone or voicemail. These verbal orders should be transcribed into the patient’s medical record or onto a prescription pad as they are being communicated. Nurses can be held responsible if they transcribe or carry out an order as it is written or if they suspect something is wrong. For instance, entering “hyper” instead of “hypo” or vice versa, and typing “he” instead of “she” are common EHR-related transcription mistakes. Outsourcing medical transcription is a feasible strategy when it comes to avoiding such documentation errors. As they are knowledgeable about medications, terminology, and procedures, experienced medical transcriptionist can detect and avoid such mistakes. They will only use abbreviations that are on the hospital’s approved list of abbreviations.
- 10. Illegible or incomplete records: This is another documentation disaster. Incomplete documentation can affect patient safety. Specificity and completeness in documentation is crucial to avoid legal issues as well as to ensure proper reimbursement.
Importantly, nurses should document only the facts. “Stick with what you’re seeing or experiencing versus what you feel and what you think,” said Natalia Cineas, Senior Vice President and Chief Nursing Executive at New York City (NYC) Health and Hospitals in the Arizona Nursing College article “[Because a] medical record medical record is subject to review – whether it’s by a regulatory agency or from a legal perspective,” Cineas noted.
Addressing the Challenges
Adequate training in EHR use, including drop-down menus, flow charts, and free texting, is critical to ensure quality nursing documentation.
Employers should also pay attention to nurses’ concerns about documentation. For instance, if there are different platforms where nurses need to enter the same information multiple times, it can lead to double documentation – an entry in the patient record of information that already exists. Double documentation results in wasted time and work overload.
To make charting seamless, it’s important that nursing documentation interfaces with the EMR. Relying on a medical transcription company that provides EHR-integrated transcription services can accurate and up-to-date charting that enhances nursing workflow.


