Transcribing a medication order or the transfer of information from an order sheet to nursing documentation is a crucial step in medication administration. With accurate transcription, the other steps in medication administration such as dispensing the drug and delivering the drug to the patient can be really effective. Understanding the possible errors that you may encounter while transcribing the order can help you to remain alert and further enhance your nursing transcription.
Transcribing a medication order or the transfer of information from an order sheet to nursing documentation is a crucial step in medication administration. With accurate transcription, the other steps in medication administration such as dispensing the drug and delivering the drug to the patient can be really effective. Understanding the possible errors that you may encounter while transcribing the order can help you to remain alert and further enhance your nursing transcription.
Medication errors related to transcription can be generally divided into four types such as:
- Errors from Poor Handwriting – Incomplete or illegible handwriting can lead to misinterpretation and grave mistakes. Healthcare providers adopting computerized medication records can eliminate this problem of misinterpretation. Even so, nurses and pharmacists at facilities where typed medication orders are not a common practice should carefully check handwritten medication orders, clarify they are legible and ensure they are interpreted correctly.
- Decimal Errors – Placing a decimal and zero after a whole number (trailing zero) while transcribing orders is not a good practice. It can lead to serious mistakes. For example, if you transcribe 5 ml as 5.0 mL, it might be read as 50 mL. Document it as 5 mL. Make sure that you don’t forget to place a zero (leading zero) before fractions that are less than one. For example, instead of writing .5mL, you should write 0.5 mL. Otherwise, it may be interpreted as 5mL.
- Misused Abbreviations – Take care to use abbreviations sparingly. Do not use abbreviations such as q.d, q.o.d, IU or u. Instead, you should write everyday, every other day, international unit or unit respectively. Latin abbreviations for the eyes and ears should not be used. Avoid using abbreviations such as µg (write mcg) because this is often misinterpreted as “mg”; H.S. (write out “half strength” or “at bed time,” whichever is appropriate,); and cc (write mL), because “cc” is often mistaken as “u” (units). You should also persuade prescribers to write out instructions instead of using abbreviations.
- Incorrect Dosage – Be alert when interpreting large medication doses more than 1000. Use commas for dosing units at or above 1,000 or use words (for example 100 thousand). There may be mathematical errors while calculating dosage. Double check all math calculation before entering the dosage into the nursing documentation form.
If you find a medication error, it is very important to notify your nurse manager and complete an incident report, generally within 24 hours. Include the following information in that report along with any additional information specified by your facility.
- Patient information
- Location and time of incident
- Detailed description of what happened
- What was done about it
- The condition of the patient
- Your signature
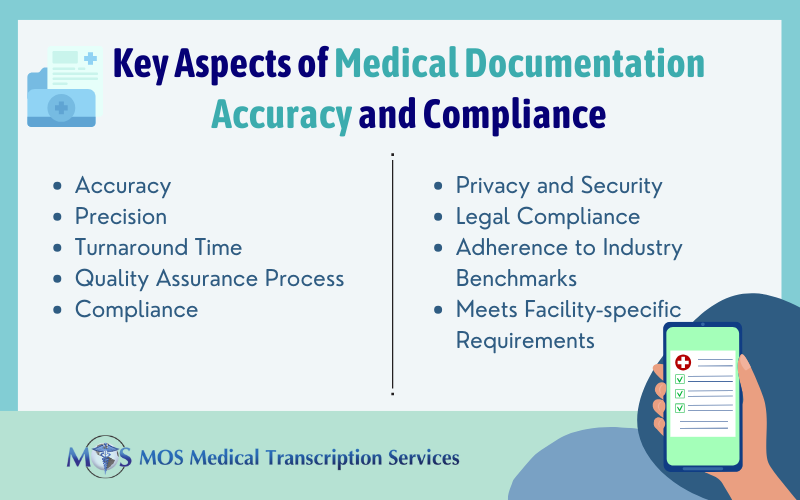
There are several factors that contribute to transcription errors including incomplete or illegible prescriber orders, lack of familiarity with drug names and so on. It is very difficult and time-consuming for nurses to check on all these factors and find solutions, especially if they are on a busy schedule. They can consider obtaining the support of medical transcription companies that offer the service of skilled and experienced transcriptionists, and have stringent QA measures in place to ensure accuracy and quality.