Patients are shifted from the intensive care unit (ICU) to a general floor when the physician determines that they no longer need such close surveillance and individualized care. Most patients and their caregivers see this decision as a step in their progress from being gravely ill to recovering. Medical transcription outsourcing ensures that the care team stays informed about the facts and circumstances related to the care provided at all stages. However, the lack of continuous or uninterrupted monitoring of vital signs when the patient is shifted out the ICU is often associated with increased morbidity and mortality. Experts point out that continuous or uninterrupted monitoring of patients transferred to general care is critical to their safety and to promote optimal outcomes. A recent www.mddionline.com report explains how a Cleveland Clinic physician is pushing for the use of technology to ensure intensivein-patient monitoring on the general care floors.
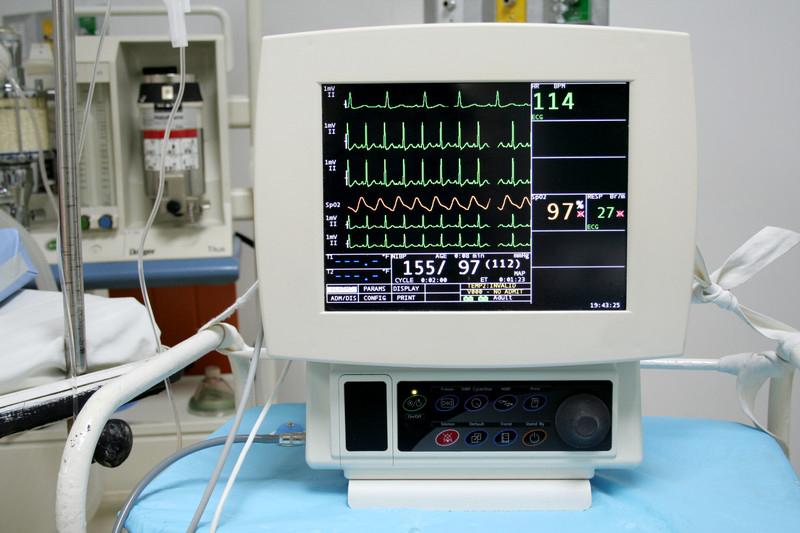
In the ICU, patients receive constant, one-to-one care from a team of healthcare professionals trained in critical care. Heart, blood pressure, and respiratory rateare monitored via machines. Ventilators may assist patients with breathing concerns until they are able to breathe naturally. Nurses report any deviations to the attending physician so that appropriate interventions can be implemented. One-to-one nursing care and 24X7 monitoring of vital signs ensures patient safety.
When ICU patients are transferred to the general wards, it signifies that their condition is improving and they no longer need the specialized care of the ICU team. Nurses perform vital check routines and monitor the patient’s condition in the general ward too, but only every four to six hours.
Monitoring only at extended intervals can lead nurses to miss signs of patient deterioration and imminent complications. For instance, they may miss symptoms of a drop in the oxygen levels in the blood, the condition known as hypoxemia. Studies have shown that respiratory failure, especially in unmonitored settings, is one of the most serious problems in hospitalized patients recovering from noncardiac surgery. Unlike critical care where continuous monitoring of respiratory function reduces the risk of undetected hypoxemia, patients in general care are seen only in a “snapshot of time”, with the result that signs of deterioration may be missed. Even if hypoxemia does not lead to respiratory arrest, it could be a strong sign of patient instability, affect wound healing, and lead to other serious complications.
According to Ashish Khanna, MD, an anesthesiologist and researcher at the Cleveland Clinic, physicians can monitor patients in general care better using aportable monitoring device. Khanna notes that:
- hypoxemia is very unpredictable and there is not good prediction model to understand which patients are at risk for cardiorespiratory depression
- studies show that about 40% of patients who develop the condition end up dying, according to some studies
The physician’s recently published study in the Journal of Critical Care describes the challenges associated with predicting episodes or severity of cardiorespiratory decompression in patients in general care who seem to be in stable condition. The paper also describes the protocol for an ongoing global trial using the Medtronic Capnostream 35 portable respiratory monitor that could significantly help in better monitoring to identify signs of deterioration in these patients earlier, that is, between routine checks.
The MedtronicCapnostream device is designed for monitoring in virtually any clinical setting. This portable monitor incorporates advanced technology and features designed to enhance workflow. It delivers real-time, continuous monitoring of the patient’s respiratory status by measuring end-tidal carbon dioxide (etCO2), pulse oximetry (SpO2), respiration rate (RR), and pulse rate. All of these variables are incorporated into a single number and displayed on a scale from 1 to 10, with 10 indicating a normal respiratory status. The ongoing global trial using the Medtronic device is aimed at deriving a risk prediction score for respiratory depression (RD) on the general care ward.
The data provided by the study is expected to reveal patterns:
- To determine real-time predictors of which patients are likely to experience respiratory depression
- When they might experience it, and
- Which patients should receive more intensive monitoring than the current standard of care
“In the end, nothing speaks like hard data. My hope is that once we’re able to prove that there is a prediction model that can be effectively used to understand who needs more intensive monitoring and then we can ultimately show that it’s cost effective, we will hopefully move in that direction,” says Khanna. He visualizes a future when hospitalized patients would wear the compact smart device so that they can be continuously monitored through surgery, through their stay in the hospital, and possibly even after they are discharged.
In addition to enhancing patient safety and care, continuous contact-free patient monitoring can also save money. HIT Consultant reported on a study published in Critical Care Medicine which suggests that improved patient monitoring can save the US healthcare system up to $15 billion annually. In this study too, the researchers describe how technology can save the day. The researchers found that hospitals implementing the EarlySense tool enjoy higher cost savings through clinical improvements. The system leverages Big Data and advanced algorithms to empower clinical staff in general wards to detect patients’ deterioration early by following and analyzing the patients’ vital signs and motion. This allows them to improve clinical outcomes and proactively reduce length of stay in the hospital’s unmonitored wards and in the ICU. This also reduces risk of adverse events such as pressure ulcers and falls and helps avoid cardiac and respiratory arrests.
Regardless of whether patients are in critical care or in the general ward, outsourcing medical transcription to an experienced service provider can ensure that the events of the patient encounter are captured accurately and that the electronic health record (EHR) properly reflects the services that were provided.


