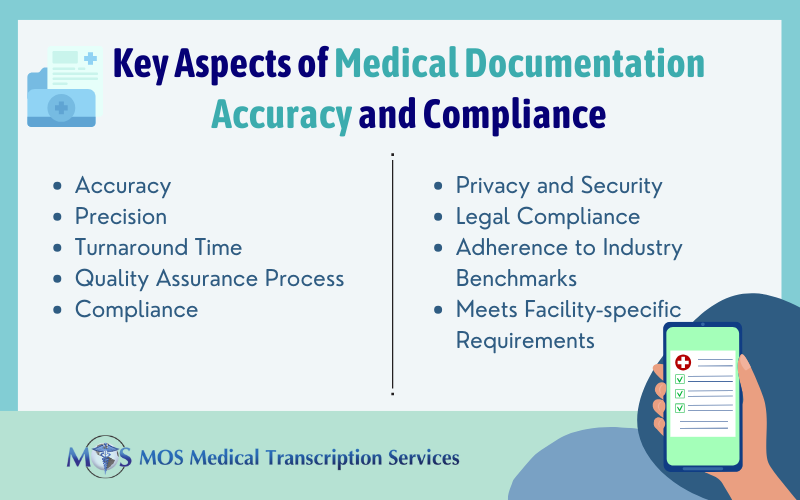
When a doctor listens to patients and takes care of their concerns, it makes patients feel more comfortable in clarifying their doubts. This helps in enhancing communication and building trust among patients. A good doctor – patient relationship is essential for providing better patient care and doctors should have sufficient time to spend with each patient. To ease the documentation workload and free up valuable time, physicians can consider utilizing medical transcription services from a reliable service provider. Physicians can also feel relaxed knowing that an experienced team is taking care of all their documentation requirements.

Communication Issues
Doctors must be better listeners if they are to provide personalized care for their patients. Most physicians are striving to achieve this and building a stronger relationship with their patient community. However, problems still exist.Often, patients are confused or do not understand what the doctor says. This is because of problems such as insufficient health literacy, inadequate patient education, and difference in cultural perceptions. Healthcare communication involves a lot of medical terminology that laymen may not understand.
Limited health literacy is a very serious concern as it can affect health status and health outcomes. The entire health system relies on the assumption that patients can understand complex medical information. If they do not understand health information, they cannot take necessary actions for their health or make appropriate health decisions. Poor health literacy among the public is the kind of weak link that can defeat even the best healthcare system. This puts an additional responsibility on physicians – they must make sure that the patients understand what they are being told. Just providing instructions may not be enough. This can be more efficiently done if the doctor can successfully build a good relationship with the patients. In cases where medications need to be changed, reduced, or increased, physicians must ideally discuss the same with the patient (if it is clinically feasible), and with the patient’s surrogate decision maker who may be a family member, or others involved with the patient.
When Patients Don’t Understand
Sometimes doctors unintentionally use words that are unfamiliar to their patients, without realizing that the meaning is not clear. It is not the patients’ fault if they don’t understand what the doctor said; when they admit they don’t understand, at least it shows that they are being honest.
When patients do not understand what the doctor said, and the doctor doesn’t pay sufficient attention or bother to explain the details again, then patients may go for a second opinion. The physician they approach could also prove confusing, and this could very well introduce a conflicting recommendation leading to more frustration and confusion. When faced with a conflicting and confusing issue, the patient may feel compelled to choose between doing nothing and following the least threatening option. Doctors should first realize this fact before launching into a discussion that begins at a level either too complex or too simple for the patient. So, what approach can doctors take?
- A good option is a technique known as teach-back, where the physician asks the patient to describe the treatment plan and corrects the misunderstood words or missing elements. This technique is proven to be effective.
- Doctors should not make the mistake of rushing through instructions at an unimaginable pace.
- Be patient and try to type out instructions that the patient can pickup when they leave.
- Make sure to simplify technical and medical terminology.
On the Lighter Side
The famous example of the diagnosis “pholenfrometry” is widely quoted on various internet sites. A patient visited his doctor after an injury. The doctor gave him some pills and wrote down his diagnosis as “pholenfrometry.” The confused patient met several specialists to understand his diagnosis and finally came back to his own doctor. The doctor replied, “You yourself told me you had “Fallen from a tree. That’s it!” So much for abbreviations!
Another inflated example of medical jargon in an emergency room is provided by Ayers Career College.
Medical jargon: Abduction was done. Perfed appy evident, secondary hemiparesis noted. Complaints of chest pain, PQRST stat.
Patient’s perception: Abduction? Ahh! I’ve been kidnapped by high-tech aliens!
Plain English: The patient needed to have a limb moved away from the midsection of his body. He has a burst appendix that is infected, partial paralysis is present. An evaluation of the chest pain will be done immediately.
(Source: https://ayers.edu/medical-jargon-appropriate-use-with-patients/)
The above quoted is a typical example of medical jargon transcriptionists at medical transcription companies have to handle frequently. Imagine how confusing and terrifying medical jargon can be to someone who has no idea of what was just said!
Misunderstanding/Misinterpretation
Language specific to certain diseases such as cancer can be very confusing for patients. A patient who was diagnosed with breast cancer in 2011 was told by her radiologist that her biopsy results had come back and they were all positive. The patient first felt relieved but then she realized that “positive” is not positive in the world of cancer. In “Cancerland” you want “negative” results, not “positive.” Another confusing word is “unremarkable” with reference to body parts. This patient says her “uterus was unremarkable” according to her scans and she thought at first that it was a “snide jab” from some lab technician until her doctor explained that it just meant there was no sign of cancer. She goes on to say humorously that “cancer isn’t just positive, it’s also remarkable.” The meanings for many words are mixed up in cancer treatment terminology – “positive,” “negative,” “progression,” and more.
Another example is that of a cancer patient who was told she was “triple negative.” She thought it meant the doctor had tested her again and again and again and it had come up as “no cancer three times.” Yet again, a man who was diagnosed with lymphoma said he was completely thrown off by the term “aspiration biopsy.” His inference was that “if it’s aspirational, it can’t be that bad.”
Building a Good Patient – Doctor Relationship
It is important to treat the patient well and at every stage the physician should explain about the treatment, medications, tests etc and keep the patient informed about the possible consequences. Physicians should focus on building a robust relationship with their patients. In other words, patients should be able to confide in their doctor and reveal their worst fears and concerns. If the doctor says something confusing, patients should feel free to request the doctor to clarify their doubts. This kind of warm and strong bonding will also help improve health outcomes and encourage patients to pay more attention to their health.
Patience and time – both these are vital for doctors to establish a strong relationship with their patients. With the introduction of EHR, doctors are forced to spend a large part of their time on medical documentation. Most physicians complain of having only less time to spend with patients. Medical transcription outsourcing to a good medical transcription company is a practical option that would reduce physician workload. This will ensure that doctors have sufficient time to communicate with their patients and establish a stronger, healthier relationship.