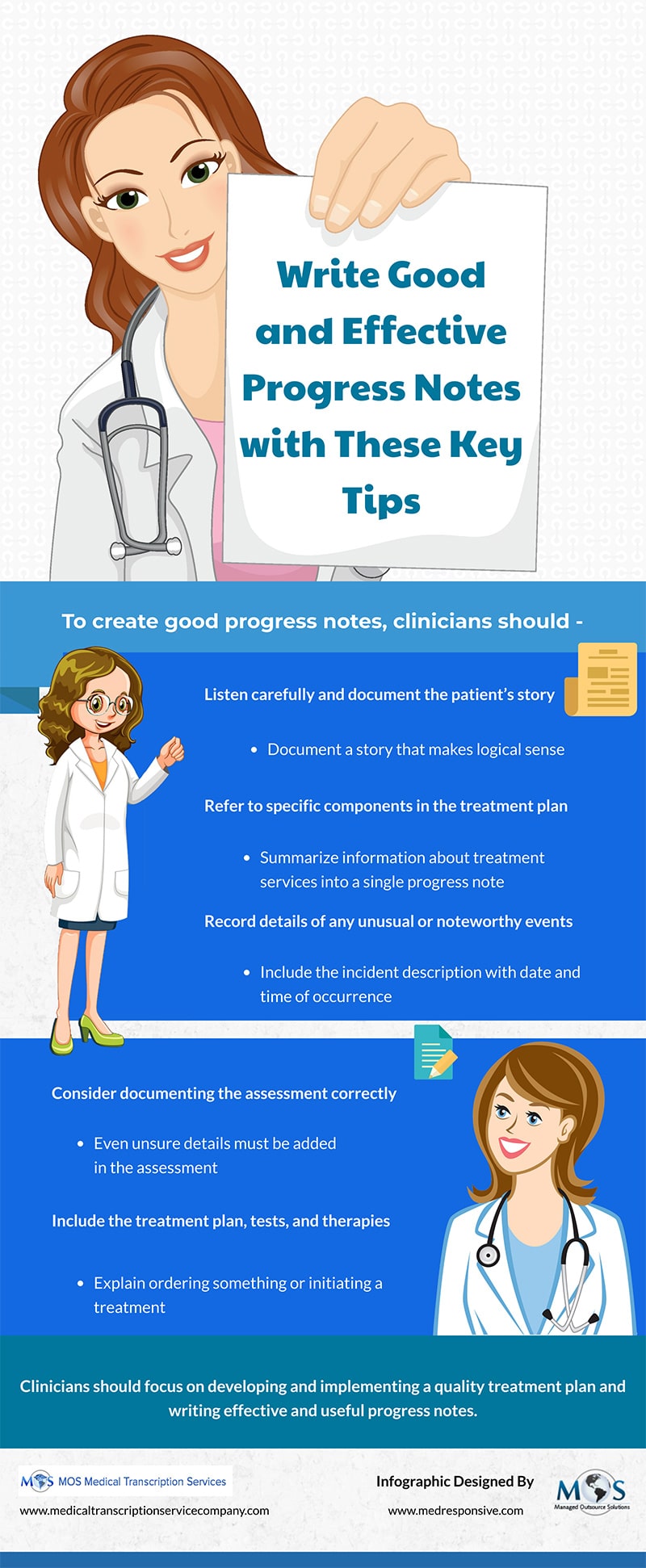
Progress notes or SOAP (Subjective, Objective, Assessment, Plan) notes, document various aspects of the patient’s treatment and highlight important issues or concerns relating to care. Good progress notes tell the patient’s story and prioritize patient care and safety. These notes provide information related to medical decision-making, patient-provider communication, critical thinking, billing and coding and medico-legal requirements for documentation. Medical transcription outsourcing is an ideal way to ensure EHR-integrated progress notes that are focused, concise, readable, organized, and useful.
Check out the infographic below
![Radiology Transcription Challenges Practices Face [INFOGRAPHIC]](https://www.medicaltranscriptionservicecompany.com/wp-content/uploads/2024/05/radiology-transcription-challenges-practices-face.webp)
![Medical Record Documentation Requirements For Podiatry [INFOGRAPHIC]](https://www.medicaltranscriptionservicecompany.com/wp-content/uploads/2023/05/medical-record-documentation-requirements-for-podiatry.jpg)