Table of Contents
Accuracy is everything in healthcare, especially when patient care depends on the information recorded in medical reports. That’s why understanding the serious medical transcription errors that can occur is so important for providers who rely on medical transcription services every day. Serious documentation errors aren’t just minor slip-ups–they are mistakes that can lead to miscommunication, delayed treatment, or even incorrect diagnoses if not caught early.
In a fast-paced clinical environment where physicians dictate large volumes of information, even the smallest inconsistency can snowball into a major issue. By understanding what can go wrong, healthcare professionals and transcription teams can work together to improve overall clinical transcription accuracy and create more reliable, error-free records that support better patient outcomes.
What Causes Serious Medical Transcription Errors?
Medical transcription is a critical part of clinical documentation, but like any process that depends on human input, it isn’t immune to errors. Even when physicians use Speech Recognition (SR) tools or dictate directly, the resulting text still needs careful review. Medical documentation must be checked for syntactical issues (how words are ordered), semantic problems (what words mean in context), misuse of jargon, and technical mistakes. When these elements are overlooked, accuracy suffers — and that’s exactly where transcription errors begin.
- Poor audio quality, including muffled or unclear recordings, makes it difficult for transcriptionists to identify important details.
- Failure to follow proper formatting standards can make even accurate information appear confusing or misleading.
- Lack of experience or limited knowledge of medical terminology increases the likelihood of errors, especially with complex terms, procedures, or drug names.
- Similar-sounding words with different meanings (homophones) can easily be confused in transcription.
- Transcription proofreading errors occur when subtle mistakes go unnoticed during documentation quality assurance checks.
- Fatigue from long hours of focused listening and typing can reduce accuracy and attention to detail.
- Background noise in recordings can interfere with clarity and comprehension.
- Differences in dictation styles, speech speed, and accents among healthcare providers create additional challenges for transcriptionists.
Serious Medical Transcription Errors to Watch Out For
Medical transcription errors can affect patient safety, treatment accuracy, and the overall quality of healthcare documentation. While some mistakes may seem minor, they can create serious risks when they involve medication details, patient identity, or clinical information. Understanding the most common errors helps healthcare providers maintain high standards and reduce avoidable risks.
- Entering Wrong Information
One of the most serious mistakes in medical transcription is entering incorrect information. This can include:
- Wrong dosage – Writing 10 mg instead of 100 mg can lead to underdosing or overdosing.
- Incorrect medical terms – Typing “hypertension” instead of “hypotension.”
- Wrong patient details – Mistakes in birth dates, allergies, or medical history.
- Incorrect unit conversions – Mixing up grams and milligrams.
- Decimal errors – A misplaced decimal can completely change a medication amount.
These errors often occur when dictation is unclear, when a physician speaks too fast, or when similar-sounding words make it hard for the transcriptionist to distinguish the correct term. Typos, fatigue, and inadequate proofreading are also common causes. Since wrong information directly affects patient care, accuracy in this area is essential.
- Patient ID Mistakes
Another serious error involves patient identification. Each patient has a unique ID number, and even a small mix-up can cause major problems. This type of mistake is especially dangerous for patients who cannot communicate clearly, patients with dietary restrictions, or those undergoing multiple tests and treatments. Incorrect identification can also lead to medical identity theft and data integrity issues.
Some transcription platforms automatically insert patient names, but others require manual entry. To avoid confusion, the transcriptionist must ensure that the dictated name matches the name on the report. If the name is missing, it must be added correctly before finalizing the document.
- Missing or Omitted Dictation
Omission errors occur when parts of the doctor’s dictation are left out of the transcript. Missing information about symptoms, diagnoses, or treatment plans can result in an incomplete and potentially misleading document. These omissions usually happen when difficult words are skipped or when the transcriptionist prioritizes speed over accuracy.
To prevent this, every word in the audio should be captured, and unclear terms should be tagged for review rather than omitted. Accuracy should always come before speed, especially when critical medical details are involved.
- Confusion in Medical Terminology
Medical terms are often complex and sound similar to one another, making them easy to confuse. Examples of confusing pairs:
- Sac / Sack
- Perfusion / Profusion
- Cord / Chord
- BNP / BMP
- Pharynx / Phalanx
- Dysphagia / Dysphasia
New transcriptionists are especially prone to these errors if they lack strong knowledge of medical terminology.
Accurate transcription requires familiarity with medical terms, abbreviations, and context. Experienced transcriptionists rely on their training to catch these subtle differences and ensure the final document reflects the correct meaning.
- Spelling Errors
Spelling mistakes can change the meaning of medical reports and create confusion. Terms like “abscess,” “syncope,” or “humerus” are often misspelled, leading to misunderstandings in clinical documentation. While electronic spell checkers can help, they may not recognize newly introduced medical terms, devices, or medications—so these must be flagged for manual verification.
- Incorrect Verb Usage and Back Formations
Some transcripts contain improper verb forms or back formations. Even though they may be used casually in everyday language, terms such as “to dehisce” or “to diurese” are not acceptable in medical documentation. Ensuring proper grammar, verb usage, and terminology is essential for maintaining clarity and precision in patient records.
Real-life Case of a Medical Transcription Error
A powerful example of how dangerous a transcription mistake can be was highlighted in an article published by a Wisconsin law firm. The case involved a diabetic patient who required insulin. She was transferred to a care facility that did not have quick access to her full medical records and instead relied on a summary dictated by the treating physician at the hospital. The physician had instructed that she receive 8 units of insulin, but the transcription service mistakenly recorded the dosage as 80 units. Tragically, the patient was administered the incorrect amount and died as a result of the overdose.
When the case went to trial, the seriousness of the error was clear. The jury deliberated for only an hour before reaching a verdict, awarding the plaintiff $140 million in damages—twice the amount requested by the attorney. This heartbreaking incident underscores the critical importance of accuracy in medical documentation. Medical information often passes through multiple hands, and even a single typographical error can lead to severe injury, life-threatening complications, or death. In this case, one misplaced digit cost a patient her life, showing just how vital precise transcription really is.
Five Tips for Avoiding Transcription Mistakes
Now that we’ve explored the most common medical transcription mistakes and the impact they can have, let’s look at practical ways to prevent them and maintain accuracy in every medical document.
- Proofread Everything Twice: One of the most effective ways to avoid mistakes is thorough proofreading. Review the completed transcript once, and then review it again. Focus on one type of error at a time such as spelling, punctuation, or terminology, to ensure a cleaner result. Reading the text out loud or even reading it backward can help you catch mistakes that your eyes may miss.
- Invest in High-Quality Audio Recording Equipment: Many transcription errors stem from unclear or low-quality audio. Using reliable recording equipment can significantly reduce misheard words and missed information. Consider using an external microphone instead of a built-in one, a lapel mic connected to your phone, a landline instead of a mobile phone, or a high-quality voice recorder. Clear audio leads to more accurate transcripts.
- Create Templates and Checklists: Templates and checklists help bring consistency to the dictation process. They offer structure and ensure that important details aren’t omitted. Providing these tools to your medical staff makes dictation easier and reduces the likelihood of missing key information.
- Disable Autocorrect: If you’re using a computer or phone for voice recording or typing, turn off the autocorrect feature. Autocorrect often makes unintended changes that lead to transcription errors. On Windows, you can disable it under Settings > Devices > Typing, and on Mac, under System Preferences > Keyboard > Text.
Work With Professional Transcription Specialists Supported by AI
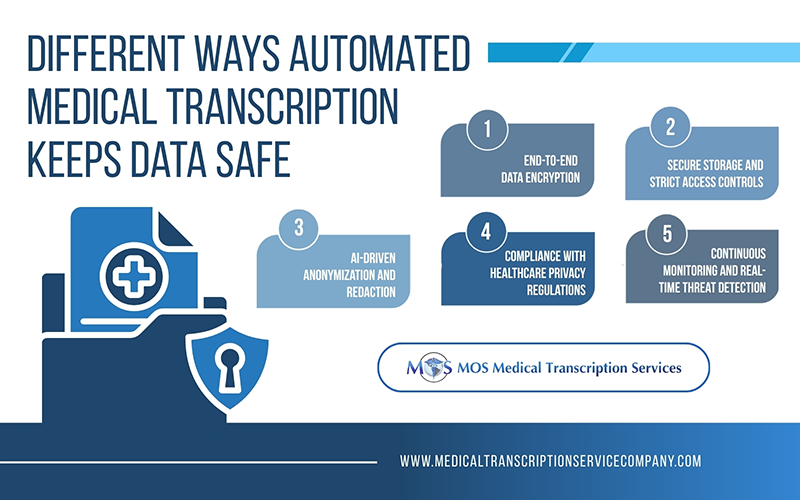
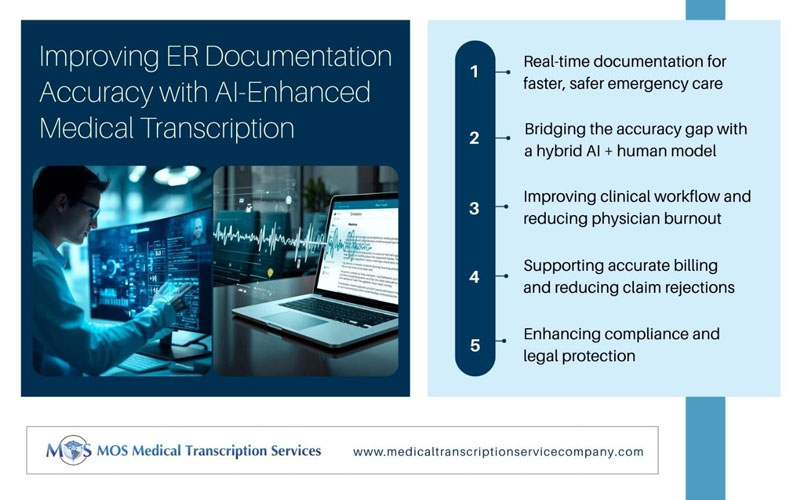
A powerful and practical way to reduce risk of transcription errors is to rely on trained experts who work alongside advanced AI-powered medical transcription tools. Professional transcriptionists bring strong language skills, deep knowledge of medical terminology, and hands-on experience in producing accurate clinical documentation. When combined with AI-driven transcription technology, their accuracy improves even further.
AI tools can quickly process recorded notes, identify key medical terms, and generate a first draft with impressive precision. Transcriptionists can then review, correct, and refine the document to ensure every detail is accurate and consistent. This human–AI collaboration dramatically reduces the chances of errors, especially in complex or fast-paced dictations.
Recognizing the most common and serious mistakes in transcription is the first step toward preventing them, and it empowers both providers and transcriptionists to pay closer attention to detail. Whether it’s misheard terms, formatting mistakes, or incorrect patient data, these issues highlight why partnering with reliable medical transcription services matters more than ever. By remaining proactive and vigilant about documentation errors, healthcare teams can ensure accurate records, reduce operational and clinical risks, and support reliable, high-quality patient care.