Discharging patients from the hospital is a complex and challenging process. Every year, over 35 million hospital discharges occur in the United States. When a patient moves from an acute care setting to other levels of care such as a Skilled Nursing Facilities (SNF), it requires efficient communication among all caregivers. This is where the discharge summary comes in. One of the important clinical reports that a medical transcription company helps hospitals create, the discharge summary provides a comprehensive overview of the patient’s hospital stay. Effective discharge summaries can reduce risk of readmission.
Table of Contents
Improving Discharge Processes Reduces Risk of Rehospitalization
Many providers and patients face communication challenges and gaps in care when a patient discharged from hospital transitions to other levels of care. This can lead to gaps in care that cause delays in care, treatment errors, unwanted procedures and potential readmissions. The Hospital Readmission Reduction Program under the Affordable Care Act (ACA) imposes penalties for unwanted hospital readmissions.
The National Guidelines recommended components of a discharge summary are:
- Patient details
- Hospital details
- Recipients
- Author
- Presentation details
- Problems and diagnosis
- Procedure
- Clinical summary
- Allergies/adverse reactions
- Medicines on discharge
- Ceased medicine
- Alerts
- Recommendations
- Follow-up appointments
- Information provided to the patient
Readmission to the hospital could be due to worsening of disease or new conditions. In many cases, new medication routines or lifestyle changes after being sent home can increase the chance of returning to the hospital.
Approximately 15% of elderly patients are readmitted within 28 days of discharge, according to a study published in Future Healthc J in 2019. The study discusses the short-term risk (within 30 days) and longer-term risk (within 180 days) of hospital readmission for older Americans who have recently had major surgery.
A recent Yale study reported that older Americans had an increased risk of hospital readmission within 180 days of undergoing major surgery, and that this risk was more acute for people who are frail or have dementia. A previous study by the same Yale team noted that that discharge summary quality was associated with hospital readmission.
A 2021 study published online in Cancer Rep (Hoboken) found that while most discharge summaries met the national guidelines quite well by including most of the recommended components, they still lack quality in some areas. The researchers referenced studies which had found that delayed, incomplete discharge summaries or discharge summaries carrying incorrect information led to increased risk of rehospitalization, complications due to medication error, morbidity and mortality.
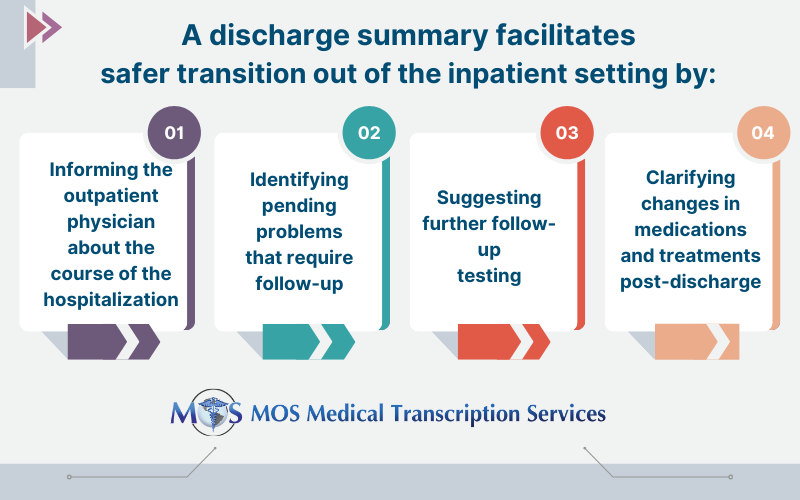
Good discharge summaries alleviate these issues by making reliable and timely patient context available. They address communication issues that can occur when patients leave the hospital, ensuring effective and timely care post-discharge. Medical transcription services play a key role in helping healthcare providers craft effective discharge summaries that meet recommended guidelines.
Outsource Medical Transcription and Ensure Effective Discharge Summaries
An experienced medical transcription service provider can ensure comprehensive discharge summaries that include all the major components, promoting continuity of care and reducing risk of complications:
- Reason for hospitalization – helps subsequent providers understand the reason why the patient was admitted to the hospital.
- Procedures performed – procedures, tests, or treatments the patient received during the hospital stay.
- Medications – new/changed medications the patient should take after leaving the hospital.
- Follow-up plans – recommended follow-up appointments, tests, or therapies
- Patient education – instructions given to the patient on dietary changes, activity restrictions, or warning signs to watch for.
Discharge documentation should include this comprehensive information. This will enable the patient’s primary care provider and other caregivers to better manage the patient’s post-discharge care, reducing risk of rehospitalization.
| Outsource medical transcription and save time and money!
Contact us today!
|


