The transition from paper charts to electronic health records (EHRs) has dramatically changed the way patient care is provided. EHRs help clinicians document treatment decisions, order medications and review laboratory results. Medical transcription companies have evolved along with the technology, helping physicians improve notes and complete patient records correctly and in a timely manner. However, while digital health records offer many benefits, interoperability depends on their capability to accurately match patient information.

Patient matching means knowing with certainty that information in the medical record belongs to the correct person. Patient matching challenges occur when:
- the physician cannot access a patient’s medical record
- the record contains another patient’s data, or
- the record contains incomplete or inaccurate information
Despite the advancements that have been made, recent reports indicate that the patient matching problem is continuing to dog the healthcare industry.
Patient matching errors can have dire consequences for patient safety. When a physician cannot access a patient’s medical record, the record contains another patient’s data, or the record contains incomplete or inaccurate information, the physician cannot provide the correct treatment. ECRI’s Patient Safety Organization says 181 healthcare organizations voluntarily reported 7,613 wrong-patient events over a 30-month period in 2013 to 2015. Lack of data integrity also leads to denied claims and wasted time, and affects patient satisfaction.
Matching patients with their records correctly has become more challenging as patients now have an increasing number of ways to enter health systems’ networks, according to an article in the Wall Street Journal. The reasons for duplicated or inappropriately merged records include:
- Typos
- Data entry errors when entering patient information initially
- Common and similarly spelled names
- Missing information
- Not updating data such as names, addresses and other identifying information
- Workarounds
- Different EHR systems record patients’ addresses in different ways. For inctance, one system may use “Street” in addresses, while others may use “St.
According to a report from Pew Charitable Trusts, as many as one out of five patients may not be matched to all the right records held at their provider.
A 2016 Ponemon Institute survey of more than 500 respondents showed that 86 percent had experienced or known about a medical error that occurred because of patient misidentification. The survey identified the following reasons for patient matching errors:
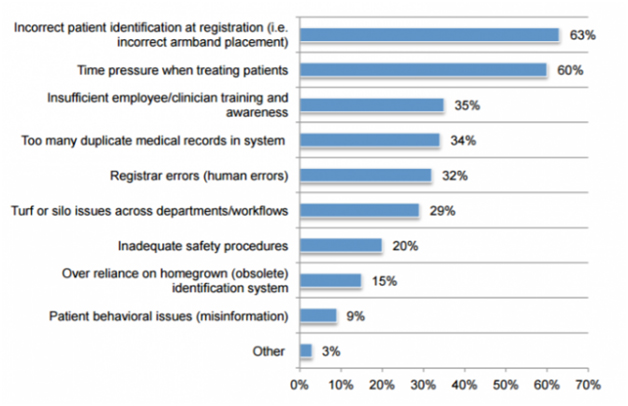
Source: www.healthitanalytics.com
In the above-mentioned survey, up to 84% of respondents said that staff had to spend about one hour to correct a patient identification error.
In January 2018, the U.S. Government Accountability Office (GAO) reported that efforts to accurately match patient records will continue to challenge providers, payers and others, with no one-size-fits-all approach to ensuring that information in different health records refers to the same patient (www.healthcaredive.com). Interoperability – linking electronic patient medical records across institutions and time – cannot succeed unless an individual’s charts held in the different places can be matched.
The GAO report discussed the various approaches that stakeholders used to identify and verify records refer to the same patient. Some used manual matching which involves manually verifying records to see if they refer to the same patient. Others reported using digital tools and software to verify data in EHRs. Based on demographic data elements, such as a patient’s name, address, Social Security number (SSN), and birth date, algorithms identify the likelihood that a given record matches a given individual.
However, stakeholders pointed out that not every system uses the same number or type of variables, and all providers do not have a sufficiently high level of data integrity to provide these algorithms with the information they need to ensure accurate results every time. Further, the GAO report stated that stakeholders said that it is difficult to determine the accuracy of the health IT tools used to match patients’ medical records automatically.
Nevertheless, both the GAO and Pew studies concluded that “no one solution currently exists to achieve highly reliable matches for all patients across all EHR systems” (www.healthcaredive.com). Solutions put forward to securely match patient records include: clarifying government funding restrictions for unique patient identifiers, reaching a consensus on standardized demographics, using apps to share identity information, verifying a patient’s phone number with the provider, and exploring the use of biometrics.
Many hospitals are already turning to biometrics to overcome a growing patient-identification problem, according to a recent WSJ article. Biometrics includes such as fingerprinting, facial recognition and iris scan. Northwell Health, based in New Hyde Park, N.Y., introduced a biometric system using iris scanning and facial recognition technology last September. The Harris Health System, which serves Houston and other areas, initiated palm-vein scanning in 2011 to identify patients. This system has nearly 2500 patients named “Maria Garcia”, and 230 of those people also share the same birth date.
As providers explore measures to ensure accurately match information in the medical record to the right patient, outsourcing medical transcription to an experienced service provider can ensure quality clinical documentation. Error-free medical records are necessary to support accurate, efficient and meaningful exchange of clinical data or interoperability.


