Table of Contents
- Medical Transcription for Faster and More Efficient Billing and Coding
- How Accurate Documentation Supports Billing and Coding
- Collaboration between Transcriptionists and Coders
- Preventing Coding Errors With Clear Medical Records
- Seamless EHR Integration for Faster Workflow
- Tracking the Impact on Revenue Cycle Performance
- How AI-integrated Medical Transcription Improves Billing and Coding
In today’s healthcare environment, clean and accurate documentation is essential for timely reimbursements. This is where medical transcription services become a crucial part of the revenue cycle. By turning spoken clinical notes into clear medical documents, transcription creates a strong link between patient care, coding, and billing. Healthcare providers can utilize medical transcription for faster billing and coding and ensure that they submit claims with fewer errors and receive payments more quickly. Accurate transcription strengthens overall healthcare documentation accuracy, ensuring the right details reach billing teams.
Healthcare teams may underestimate how inaccurate or unclear documentation can slow down reimbursements. Coders struggle to assign the right ICD-10 and CPT codes, claims get denied, and staff spend extra hours correcting small but costly mistakes. A reliable transcription workflow eliminates many of these issues, allowing your practice to get paid faster and maintain steady financial health through billing process optimization.
Medical Transcription for Faster and More Efficient Billing and Coding
The accuracy of your documentation directly affects how quickly your claims are processed. When a transcriptionist carefully listens to a doctor’s dictation and converts it into a structured, well-organized report, coders can work more efficiently. They don’t have to guess procedures, interpret unclear wording, or track down missing details. By improving healthcare coding accuracy with transcription, you can speed up the claim cycle and get the due reimbursement.
How Accurate Documentation Supports Billing and Coding
High-quality transcription plays an important role in ensuring the correct codes. Coders rely heavily on clear terminology, complete descriptions, and essential clinical details. When any of this is missing, errors are more likely. That leads to:
- Claim delays
- Denials
- Lost revenue
- Extended accounts receivable cycles
A detailed transcript eliminates these issues. For example, including information about laterality, procedure modifiers, dosage, or follow-up instructions helps coders apply the proper codes with confidence. When a transcriptionist flags unclear statements, coders save time and avoid unnecessary audits. As a result, claims move through the system quickly, reducing the overall payment cycle and offering consistent medical coding support for billing teams.
Collaboration between Transcriptionists and Coders
Better communication between transcriptionists and coders can significantly improve documentation quality. When both teams have ongoing feedback loops, they begin to understand each other’s challenges. Coders can point out recurring issues-such as missing modifiers or confusing terminology-while transcriptionists can ask for clarification when the dictation lacks detail.
This teamwork provides the following benefits:
- Fewer coding queries
- Less back-and-forth communication
- More complete patient records
- Faster bill processing
Over time, both departments learn to anticipate each other’s needs. This makes the workflow smoother and reduces the chances of costly mistakes in billing.
Preventing Coding Errors With Clear Medical Records
Many coding errors begin with unclear handwritten notes, missing patient information, or inconsistent terminology. Transcription helps eliminate these problems by offering clean, standardized, and well-structured documents.
A trained medical transcriptionist is skilled at catching inconsistencies the provider may not notice, such as:
- A misplaced decimal in medication
- Missing follow-up instructions
- Unclear abbreviation that could lead to miscoding
Insurance companies reject thousands of claims each year due to avoidable documentation mistakes. By ensuring accuracy upfront, transcription reduces denials and protects your revenue stream. Every corrected detail helps your billing department work faster and with more confidence. So, providers should consider accurate transcription for faster claim reimbursements.
Seamless EHR Integration for Faster Workflow
Today, most practices rely heavily on electronic health record (EHR) systems. When transcripts integrate smoothly with your EHR, the billing team can easily pull information into their coding tools without manually re-typing data.
This offers several key benefits:
- Lower risk of typing errors
- Faster billing turnaround
- Less administrative burden on staff
- More consistent patient records
- Better compliance with HIPAA and security standards
When everything flows automatically from transcription to coding to billing, your team can focus on patient care instead of documentation. This improves overall operational efficiency and accelerates claim processing.
Tracking the Impact on Revenue Cycle Performance
One of the most effective ways to understand the value of medical transcription is by tracking key revenue cycle metrics. Practices that upgrade their transcription workflow notice improvements in:
- Days in accounts receivable
- Number of denied claims
- Time spent reviewing charts
- Billing team productivity
- Reimbursement speed
Conducting a simple before-and-after audit can reveal double-digit improvements in claim acceptance rates. Clearer transcripts lead to fewer errors, fewer resubmissions, and far less administrative stress.
How AI-integrated Medical Transcription Improves Billing and Coding
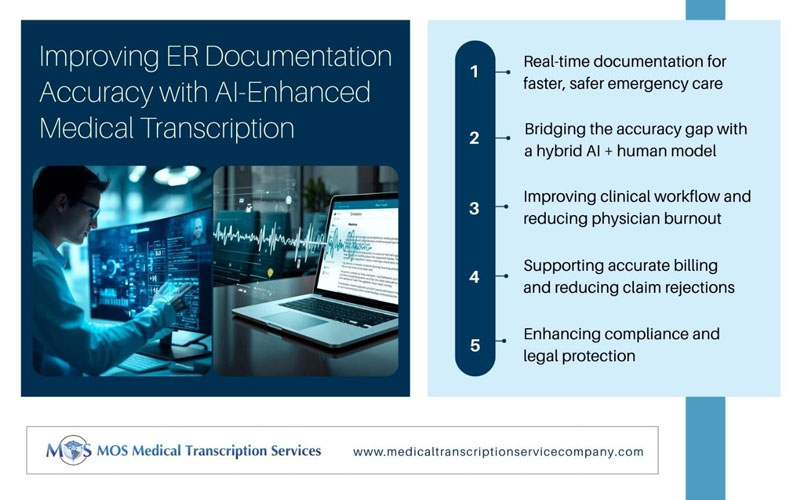
AI-powered transcription tools are adding an extra level of support for billing teams. They help detect missing clinical details, flag unclear dictation, and ensure terminology is consistent. AI can also identify patterns in coding errors and suggest improvements. When combined with human review, this hybrid model ensures more accurate records, fewer denials, and faster payments. For many practices, AI-assisted transcription has become an essential tool for improving billing efficiency.
Accurate documentation is the foundation of effective coding and billing. By investing in reliable medical transcription services, healthcare providers can reduce coding errors, speed up claims processing, and maintain stronger financial stability. A clean transcript not only supports proper patient care but also drives smoother reimbursement workflows. When you strengthen your transcription process, you strengthen your entire revenue cycle—giving your practice the clarity and accuracy it needs to get paid on time.