
Precise and timely documentation of patient records is critical in the healthcare sector. Medical transcription is essential for turning physician dictations and other audio recordings pertaining to healthcare into accurate medical records and promote efficient communication among healthcare practitioners. The information contained in a patient’s medical records is essential for providing the right kind of treatment. When prescribing medication, medical professionals rely on this information to guide their decisions. Ensuring the completeness of the records is crucial. To help the patient receive more care, these records are frequently referred to experts and other medical facilities. Due to rising demand for quality medical records more medical organizations are using medical transcription services which increase the productivity of documentation entry and ensure patient safety.
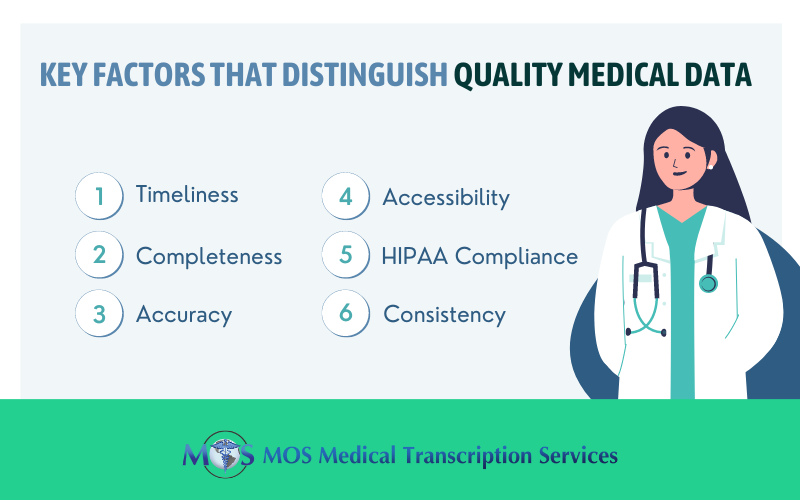
Features of Quality Medical Data
Let’s look into the essential characteristics of medical data and the various measures that health care providers need to adopt to ensure quality.
- Timeliness: Timeliness means that the data should be recorded within an appropriate time frame, typically as it is being collected. If the nurse monitors a patient at 5 pm, the note in the patient record should be written soon after that and preferably at the point-of-care. Surgeons need to record operative notes shortly after the surgery and not weeks later.
According to The Joint Commission’s 2012 accreditation standards, an operative report must be documented immediately after the operation. The Federal Register (2012) recommends that a history and physical must be dictated and present in the health record within 24 hours of admission or before an operation. The Joint Commission and Conditions of Participation (COP) standards recommend that following a patient’s discharge from an acute care facility, the record must be completed within a specified time, usually 30 days. If state licensing law recommends a shorter time frame, this should be given precedence.
Medical transcription service companies play an important role in ensuring timely medical documentation by providing transcripts of healthcare providers’ dictation in custom TAT. They also offer several convenient options for dictation such as toll-free phone-in, digital recording, smartphones and conference calls.
- Completeness: Complete data is necessary to support patient care. Completeness refers to collection or recording of all relevant medical data including vital signs such as blood pressure heart rate, respiration rate, temperature, neck and head exam, neurological exam, dermatological exam, and physical and sensory changes. A record would be considered incomplete if any vital sign or data had been missed out and if the time and date has not been entered. For a progress note to be complete, it must be authenticated.
- Accuracy: This means avoiding errors in data entry. An article published by Modern Healthcare in February noted that electronic health records (EHRs) are breeding grounds for wrong data entry due to confusing computer displays. This could lead to errors such as ordering the wrong medications or missing key patient information.
In order to ensure that the data collected is timely and complete, health care providers need to develop and implement data quality controls. These include preventive controls, processing controls and corrective controls. Preventive controls refer to procedures, processes or structures developed to minimize errors at the point of data collection. Examples include software alerts when date is entered wrongly or verbally identifying the patient before taking a blood sample. Drop-down menus in EHRs are designed to prevent invalid data entries. However, the errors can occur if the physician selects the wrong item. Processing controls help discovery of errors through quantitative analysis and error reports which highlight mistakes as well as omissions. Corrective controls involve correction of errors that have been discovered. The problem is that certain errors such as the administration of a wrong medication cannot be corrected. So the source of the error must be investigated to prevent future occurrence.
- Accessibility: The ease of communication and cooperation between healthcare providers involved in a patient’s care continuum depends on the accessibility of medical records. Secure electronic health record (EHR) systems and other approved platforms should make transcribed medical records freely available. Regardless of whether they are accessing records within the facility or remotely, healthcare providers need to be able to retrieve patient information quickly and effectively. Medical personnel can make prompt decisions, maintain continuity of care, and enhance patient outcomes by making sure that they are accessible.
- HIPAA Compliance: Ensuring patient privacy and confidentiality through medical transcribing requires adherence to the Health Insurance Portability and Accountability Act (HIPAA). To maintain the privacy of patient information found in audio dictations and transcribed documents, transcriptionists are required to abide by strict security measures and HIPAA rules. Protecting protected health information (PHI) from unauthorized access, disclosure, or misuse entails putting in place access controls, confidentiality agreements, secure file transfer protocols, and encryption technology. Medical transcription providers maintain the highest levels of patient data security and confidentiality by placing a high priority on HIPAA compliance.
- Consistency: Improving the readability and usability of medical records requires consistency in layout, language, and style. To ensure consistency among patient records and healthcare facilities, medical transcriptionists must consistently transcribe different kinds of dictations. Respecting the uniform forms, policies, and procedures set out by medical associations aids in ensuring that medical records are consistent and interchangeable. Both patients and healthcare providers gain from rapid information retrieval, data analysis, and decision-making made possible by consistent transcription procedures.
Paying attention to the key factors listed above is necessary to ensure the quality of medical records during the medical transcription process. Medical transcriptionists contribute significantly to the creation of accurate, trustworthy, and useful medical records that facilitate clinical decision-making, the best possible patient care, and regulatory compliance in the healthcare sector by adhering to these criteria. Outsourcing medical transcription is a practical option when it comes to avoiding clinical documentation errors. Reliable companies have stringent quality control measures in place to ensure documentation of physician dictation with up to 99% accuracy.


