Table of Contents
- Operative Notes Transcription and Its Role in Modern Healthcare
- What Makes an Operative Note So Important?
- How Operative Notes Transcription Supports Better Patient Care
- Why Accuracy in Operative Notes Matters
- The Process Behind Reliable Operative Notes Transcription
- Best Practices for Effective Operative Note Documentation
- AI-integrated Transcription: A Modern Add-On to Surgical Documentation
In today’s fast-paced medical environment, clear and accurate documentation is essential for delivering high-quality patient care. One of the most important documentation tools used in surgical settings is operative notes transcription. These records help surgeons, nurses, and postoperative care teams access detailed information about every surgical procedure.
When provided by professional medical transcription services, operative notes become reliable clinical documents that guide follow-up treatment, support billing accuracy, and ensure compliance. Without properly structured operative reports, communication gaps can easily arise, affecting patient outcomes and delaying essential care. Let us consider how operative note transcription improves patient care across different stages of treatment.
Operative Notes Transcription and Its Role in Modern Healthcare
Operative notes transcription involves converting a surgeon’s dictated or recorded explanation of a procedure into a structured written document. This process ensures that every detail—from what happened during surgery to what should happen in recovery—is captured clearly and accurately. Since surgical procedures can be complex and time-sensitive, having a dependable transcription workflow is essential for improving care delivery across departments. It also contributes significantly when it comes to ensuring clinical workflow efficiency, especially in busy surgical units.
These operative reports serve as a bridge between the surgical team and other healthcare professionals, helping ensure that no detail is overlooked during the transition from the operating room to postoperative care units. For many facilities, associating with operative report transcription services enhances accuracy and timeliness.
What Makes an Operative Note So Important?
An operative note is much more than a summary of a surgical procedure. It is a legally required medical record and an essential communication tool. A complete operative note usually includes:
- The patient’s medical history
- Date, time, and duration of surgery
- Type of procedure performed
- Operative findings
- Estimated blood loss
- Surgical tools, implants, or prostheses used
- Complications, if any
- Post-operative care instructions
Each of these elements plays a vital role in ensuring patient safety and continuity of care. When these notes are well-organized and accurately transcribed, surgical documentation accuracy is ensured and healthcare professionals across departments can make informed decisions quickly and confidently.
How Operative Notes Transcription Supports Better Patient Care
Accurate operative reports help improve patient care in several ways. First, they give postoperative nurses and physicians a clear understanding of what occurred during the surgery. This helps them monitor recovery more effectively, avoid complications, and follow precise instructions provided by the surgeon.
Second, clear documentation reduces the risk of miscommunication. For example, if a surgeon specifies that a patient needs a particular medication, wound care method, or follow-up test, the transcription ensures that these details are not lost or misinterpreted.
Finally, operative notes provide essential information for long-term care. If a patient returns months or years later with a related issue, surgical teams can refer back to the transcribed report to guide their decisions. These constitute the benefits of accurate surgical transcription for healthcare teams.
Why Accuracy in Operative Notes Matters
Surgical documentation must be precise. Even small errors or omissions can affect patient outcomes. Handwritten notes, rushed entries, or unclear dictation can create gaps in understanding. Accurate transcription benefits include the following:
- Correct postoperative treatments
- Smooth communication between surgical and nursing teams
- Reduced medical errors
- Better patient outcomes
- Safer care delivery
Transcriptionists trained in medical terminology and surgical procedures can capture every detail correctly. This specialized knowledge ensures that reports are complete, standardized, and easy for healthcare teams to interpret.
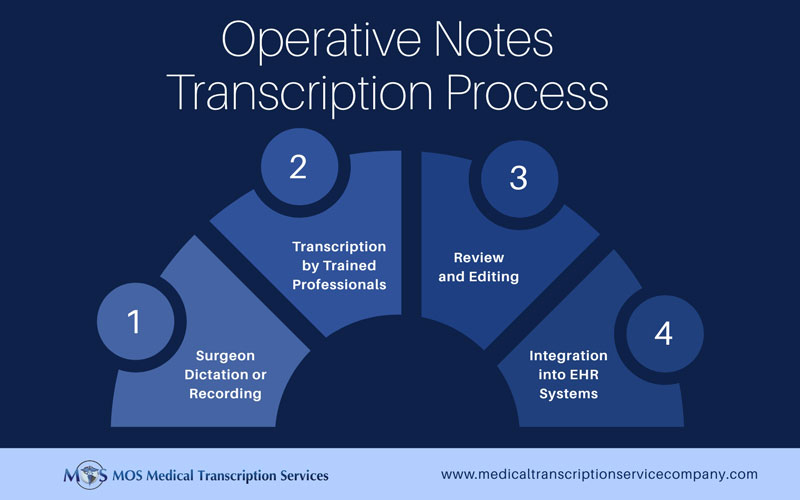
The Process Behind Reliable Operative Notes Transcription
The transcription of operative notes follows a structured process to ensure accuracy, clarity, and security.
- Surgeon Dictation or Recording: After completing the procedure, surgeons typically dictate operative details through secure digital devices. Time-sensitive information is captured while the procedure is still fresh in memory.
- Transcription by Trained Professionals: Medical transcription specialists listen carefully to the audio and convert it into a clear, formatted document. Their expertise ensures that terminology, procedure descriptions, and patient information are accurately transcribed.
- Review and Editing: Once transcribed, the document undergoes a review to check for formatting, accuracy, and consistency.
- Integration Into EHR Systems: The final report is uploaded into the patient’s electronic health record (EHR), where it becomes accessible to the entire care team for future reference.
This streamlined process helps improve communication, supports better decision-making, and enhances workflow efficiency across departments.
Best Practices for Effective Operative Note Documentation
High-quality operative notes follow standardized documentation practices. Some of the best methods include:
- Use of Standard Template: Following established guidelines ensures consistent documentation of all essential details.
- Clarity and Accuracy: Avoiding ambiguous language or hard-to-read handwritten notes reduces errors and delays in care.
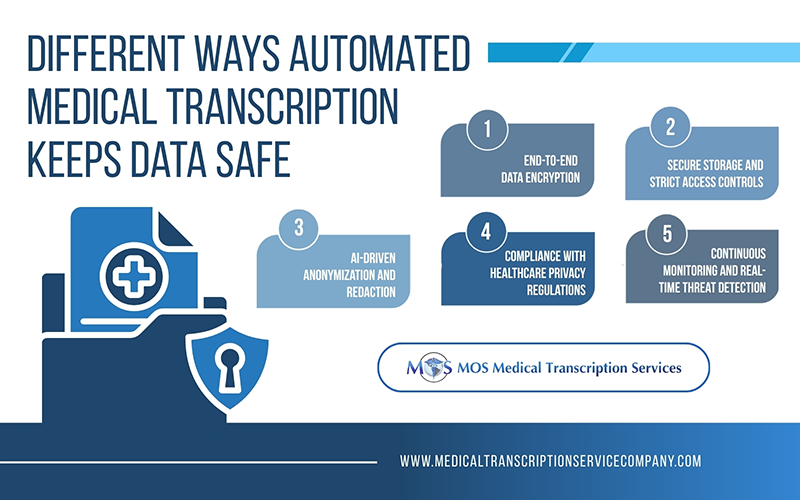
- HIPAA-compliant Methods: Secure tools and storage ensure patient privacy and confidentiality at all stages of transcription.
- Use of Modern Technology: Digital dictation tools, mobile apps, and AI-driven support systems help streamline the process and prevent documentation gaps.
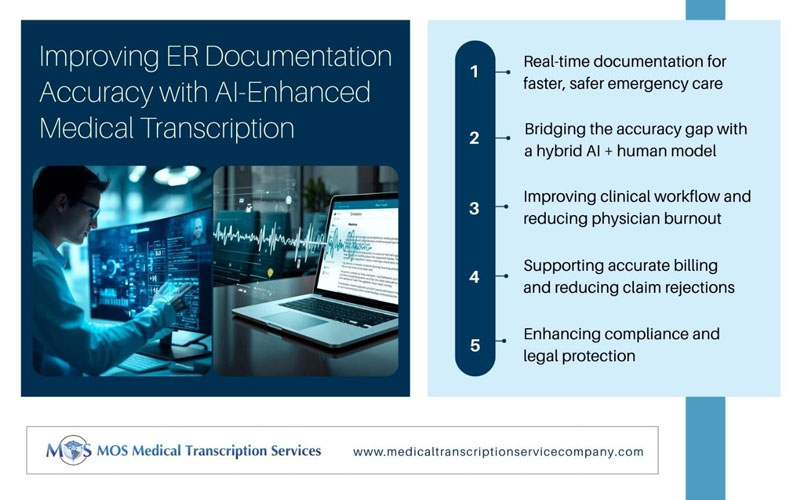
AI-integrated Transcription: A Modern Add-On to Surgical Documentation
AI-powered transcription systems are transforming the way operative notes are documented. These tools help detect unclear dictation, highlight missing details, and reduce transcription errors. When used alongside human transcriptionists, AI enhances:
- Speed of documentation
- Terminology accuracy
- Consistency across multiple operative reports
This hybrid approach strengthens billing accuracy, supports compliance standards, and improves the quality of surgical records. As a result, healthcare professionals enjoy a faster, more reliable documentation process that enhances overall care delivery.
Operative notes transcription plays an essential role in improving care delivery, enhancing communication, and supporting accurate documentation across surgical teams. By ensuring that every surgical detail is captured clearly and systematically, healthcare providers can deliver safer, more efficient, and more coordinated care. When supported by trusted medical transcription services, operative notes become powerful tools that improve patient outcomes, streamline workflows, and meet legal and compliance standards. Investing in high-quality transcription is ultimately an investment in better care and smoother operations throughout your healthcare facility.