Table of Contents
Clinical documentation is the capture of clinical information at the patient encounter. Clear, accurate, consistent, complete, timely, and legible clinical documentation is necessary to reflect the patient’s condition and provide evidence that the care rendered was meaningful and medically necessary. Behavioral health providers, for instance, are required to document many types of notes from patient to patient and meet regulatory standards of practice and maintain appropriate, HIPAA compliant documentation. Outsourced medical transcription services can help therapists overcome the challenges of maintaining good clinical documentation.
Clinical Documentation in Behavioral Health
Therapy notes describe what occurred during a session, outline the general treatment plan, provide an idea about the patient’s mental health state, and document next course of action in the treatment. Discussed below are the different types of notes maintained by behavioral health providers:
- Psychotherapy notes or process notes: Mental health professionals maintain psychotherapy notes or process notes to document the details of the conversation during a private individual, group, joint, or family counseling session. These notes cover observations, the patient’s demeanor, hypotheses about a diagnosis, thoughts and feelings about the session, and questions. Psychotherapy notes are kept separate from progress notes. These notes cannot be released without authorization and excluded from the provision that allows patients to see their health information.
- Progress notes: These notes include assessment, diagnosis, and treatment interventions, referrals, preventive services, and coordination of care with other healthcare providers. Progress notes more formal than process notes and include elements such as diagnosis, prescriptions and type of therapy with session dates and stop times, and all other components necessary for billing and reimbursement purposes. Providers should also document any unusual challenges the patient faced during the therapeutic process and how they were addressed. Progress notes must be objective, concise, relevant and well-written.
- SOAP Expanded as Subjective, Objective, Assessment and Plan, the SOAP format is a widely used format structure for progress notes. It allows healthcare professionals to capture and communicate patient information from a session in a clear, concise way. Writing proper SOAP notes can go a long way in improving the quality of care.
- SOAIGP: This format is more detailed than SOAP. SOAIGP expands to Supplementary Database Information, Observations, Activities with and on behalf of the patient, Impressions and Assessment, Goals and Plans for next actions by the worker and client.
- BIRP: BIRP – Behavior, Intervention, Response, and Plan – is another option to document a patient’s treatment and progress. It allows therapists to organize their notes into these specific sections and ensure that patients who see multiple providers to get continual care.
- DAP: DAP stands for Data, Assessment and Plan. This is one of the latest ways to write a psychotherapy or progress note. DAP notes combine the subjective and objective sections in SOAP notes into one comprehensive section. DAP notes allow therapists to quickly document individual and group psychotherapy sessions.
- Group notes: Well organized documents are necessary for family therapy and other types of group sessions. In addition to the group summary and synopsis, therapists must document identifying information and details for each participant – from mood and body language, participation, issues between group members, objectives and goals for each patient and how they can achieve them to interventions, client feedback, and plans for future sessions.
According to Catalysts Counseling, therapists can make the record keeping process easier by keeping the phrase “golden thread” in mind when documenting diagnosis, the progress note, and the treatment plan. These three elements should all link together when documenting patient interactions.
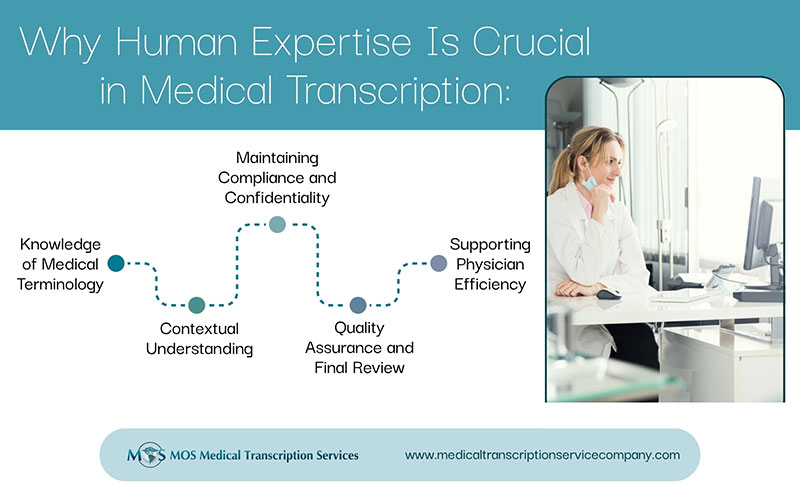
Role of Mental Health Transcription Services
As they focus on their patients, relying on a HIPAA-compliant mental health transcription service provider can help therapists maintain clear, confidential, well organized and timely clinical notes. The benefits of partnering with an experienced transcription company are:
- HIPAA-compliant documentation: When it comes to mental health, the most important principles under HIPAA are with regards to privacy, security, and breach. Under the HIPAA Privacy Rule, the following information is subject to stringent privacy regulations (icanotes.com):
- Any identifiable health information regarding the individual’s past, present or future physical or mental health
- The type of health care provided to the patient and the reasons for the type of care
- Information relating to the past, present or future payment for the care and treatment provided
All mental health documentation should remain completely confidential unless therapists are required to share it with other healthcare professionals or their patients. Partnering with a HIPAA-compliant medical transcription company can help therapists maintain good documentation. Reliable service providers have stringent regulations in place to protect the security, privacy, and confidentiality of the protected health information.
- Documentation of large volumes of records in quick turnaround time: Experienced medical transcription companies can handle transcription tasks of any volume in quick turnaround time. Therapists capture information from a variety of sources: referrals, the patient interview, additional information received from other providers and family members. Details about the patient’s appearance, emotional expression, and affect, and their reactions or interaction with the therapist during the interview should also be noted. Capturing all of this information in individual and group sessions can be extremely challenging but crucial to provide targeted therapy. Outsourcing transcription to an expert is an ideal way to deal with this.
- Accurate, detailed documentation: A thorough mental health assessment is necessary to collect all the details about a patient’s symptoms and complaints. This will enable proper diagnosis and appropriate treatment planning as well as help identify potential referral opportunities, so that the patients can benefit from the planned treatment. Qualified medical transcriptionists are familiar with the terminology, jargon and slang used in mental health services and can ensure accurate detailed documentation of mental health assessment for the medical record. This will provide the basis for the development of all other clinical documentation.
Therapy notes are at the core of the patient encounter and allow providers to track the patient’s progress till treatment goals are achieved. Medical transcription outsourcing to a HIPAA complaint company can help therapists maintain good clinical documentation that meets stringent confidentiality standards.
| MOS Medical Transcription Services has extensive experience providing customized clinical documentation solutions for all medical specialties. We can handle projects of any size in quick turnaround time. |