
Table of Contents
Clinical documentation comprises all the information relating to each patient’s encounters with a healthcare facility. This information is entered in the medical record by a member of the patient’s healthcare team – a physician, nurse, therapist, dentist or other healthcare professional. Chronologically documenting this information in the medical record is essential for the provision of continuous, high quality care. With the rising incidence of patients with chronic conditions and complexities of EHR data entry, many practitioners consider medical transcription outsourcing a reliable strategy to create proper medical records.
Today, there is an increased focus on clinical documentation improvement (CDI) to ensure accurate, quality, complete, and specific documentation that reflects severity of illness and care provided. Many providers are utilizing AI technology to create clinical documentation, reduce time spent on EHR data entry, facilitate effective patient interactions, and reduce the burden of after-hours clerical work. However, AI scribe service is here to stay, vetting by human transcriptionists is crucial to ensure accuracy.
Why CDI is Vital for Patient Care
Proper patient care depends on efficient communication among healthcare providers. As an AHIMA article notes, the patient’s condition can change abruptly, and communicating and documenting changes and resulting responses is necessary to prevent “missteps” in care. The report explains that failure to document properly can lead to the following problems for the patient:
- Being overcharged or not covered for treatment that may have been necessary
- Being wrongly categorized as being less sick because aggregated diagnoses do not reflect severity of illness
- A higher risk of developing complications of care since acuity of symptoms are not described
- Face increased chance of readmission after discharge if the appropriate treatment plan was cut short or weekend follow-through lapsed due to short staffing.
Purposes of Clinical Documentation
The medical record is the most important means of communication between members of the patient’s healthcare team. As the American Health Information Management Association (AHIMA) explains, “Clinical documentation is at the core of every patient encounter. In order to be meaningful, the documentation must be clear, consistent, complete, precise, reliable, timely, and legible to accurately reflect the patient’s disease burden and scope of services provided”.
Good clinical documentation is important for many reasons:
- Promotes continuity of care and communication among healthcare professionals involved in the patient’s care
- Shows that proper care was given and documents the patient’s response to that care
- Provides evidence for legal records
- Creates patient registry functions to manage large populations better
- Provides information for researchers conducting scientific studies
- Helps create longitudinal patient records (LEPRs)
- Enables medical coders to prepare and evaluate insurance claims
- Paper or electronic documentation needs to be supported by imaging records such as X-rays, magnetic resonance imaging (MRIs) scans, electrocardiograms (EKGs), etc.
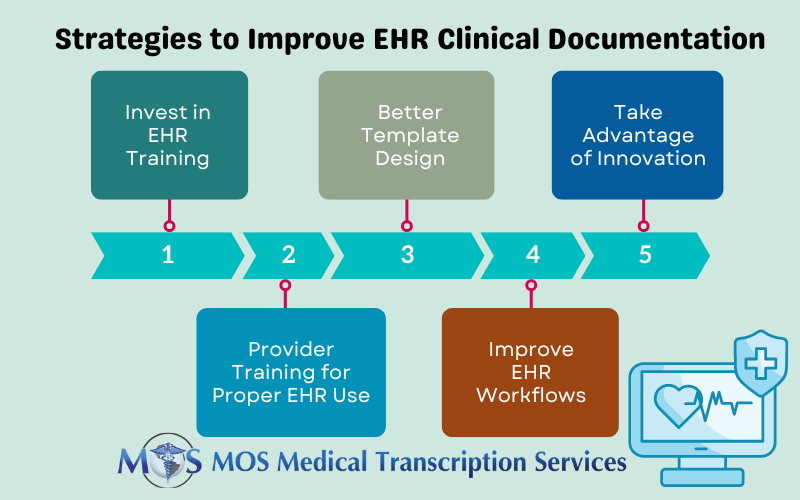
Strategies to Improve EHR Clinical Documentation and Save Physicians’ Time
- Invest in EHR Training: It is important that organizations invest in training physicians and/or nurses who use the EHR system to improve efficiency and provider wellbeing. An article from the American Academy of Pediatrics lists the three steps in the EHR training process as:
- Onboarding: This can be administrative in nature and include licensure, credentialing, creating a login account and customization of EHR interface or tools, or comprise pretests and exercises.
- Classroom Training: This involves teaching providers how to navigate the EHR efficiently, learn inpatient and/or outpatient charting and flowsheets, and practice writing short, accurate notes designed to enhance clinical care, and customize workflow.
- One-on-one Support: In this phase, a training team or an EHR-trained physician shows other providers how to use EHRs efficiently and avoid or decrease burnout. By working with groups, physicians can learn how to write clinical progress notes effectively using their EHR system.
- Reduce Payer Documentation Requirements: A study published in 2018 reported that the length of the average patient note in an EHR was 700 words – more than double that in 2009. One of the reasons for this is payer documentation requirements. Clinicians and hospitals have to report an assortment of measures to different payers. The Patients over Paperwork initiative led by the U.S. Centers for Medicare and Medicaid Services (CMS) is aimed at reducing the administrative burden on providers. The initiative has made great progress in doing away with unnecessarily complex, outdated, or duplicative requirements that consume physicians’ time while doing little to improve quality of care.
- Better Template Design: Improving EHR template design can save physician time spent on documentation. Many template designs focus on creating clinical notes to ensure efficiency at the point of care, but do not pay attention how the data is presented. Template design needs to be improved to allow physicians to spend less time on updating patient profiles and ordering exams, and more time with patients. Templates should also be designed for better presentation of data to patients, other providers, and staff for continuity of care.
- Improve EHR Workflow: Experts who evaluated EHR implementations across several organizations said that removing unnecessary steps can improve workflows in the EHR by about 20%, on average – without any regulatory changes or technology innovation (www.hbr.org). Reducing the number of clicks that physicians need to perform should be done continually as it can increase provider satisfaction and reduce time for patients to be seen.
- Take Advantage of Innovation: Huge volumes of unstructured data are inputted into EHRs on a daily basis. Advanced natural language processing (NLP) technology can provide great insights into the data and extract relevant information within the patient chart which can be used to improve the quality of care. Today, application programming interfaces (APIs) also support interoperability of EHR systems, allowing them to send or retrieve data to update a patient record.
Other Recommendations
The AAPC (American Academy of Professional Coders) defines CDI as “the process of reviewing medical record documentation for completeness and accuracy”. Clinical documentation review is performed by clinical documentation specialists who have both clinical and medical coding backgrounds. Here are some expert recommendations to improve clinical documentation:
- Plan ahead and hire efficient CDI specialists.
- Assess existing policies and procedures, including the current state of the facility’s CDI program.
- Educate clinical documentation specialists, coders, and other clinical professionals before setting up the CDI program.
- Review a sample of records to know where to focus efforts for documentation improvement and show how this will benefit the patient, practice, or population.
- Review the medical record before the encounter to assess for issues and identify compliance opportunities
- Have the CDI specialist review claims with targeted diagnosis codes before submission and determine if the documentation supports the codes. If not, the coder can reassign the codes.
- Consider the changing health care operational environment and prepare for it.
- CDI specialists should help physicians and coders work together to improve documentation.
- Utilize technology.
Benefits of Clinical Documentation Improvement
CDI is beneficial for many reasons:
- More meaningful patient information: An effective CDI program results in a more useful medical record and more meaningful patient information and data.
- Improved patient care: Proper records can improve patient care in a healthcare facility. Review of documentation by the CDI specialist enhances communication between all providers involved in the patient’s care in a timely manner. This can reduce the length of stay for the patient and also help prevent avoidable readmissions.
- Improved reimbursement: Payers often require additional documentation to support additional or more specific ICD codes to enhance hospital reimbursement and data collection. A CDI specialist can confirm patients have accurate diagnoses in the medical record by reviewing documentation and ensure comprehensive data for accurate reimbursement.
- Timely reimbursements: When there are no errors in the documentation, it can prevent delays in claims processing.
- Reduced denials: Improved clinical documentation can result in more accurate medical coding, which will reduce denials and improve the appeals process.
- Validation of care quality: By ensuring quality clinical documentation and data, CDI can help healthcare professionals meet the demands to provide evidence of the quality of care.
- Capture of accurate risk adjustment scores: Continuous capture of all chronic conditions on a yearly basis, accurate HCC coding, and identifying risk adjustment scores can lead to better patient treatments and outcomes as well as proper Medicare physician reimbursement.
- Promotes compliance: Poor documentation leads to errors in claim submissions, which can attract audits and result in fines or return of money mistakenly collected from payers. When documentation is accurate and complete, it supports compliance with regulations.
When successfully implemented, a clinical documentation improvement program can ensure accurate and thorough medical record documentation. This will improve reporting quality, promote accurate reimbursements, and drive better patient outcomes. The widespread adoption of EHRs and technologies such as front-end speech recognition has made it easier to create clinical documentation. Partnering with a medical transcription company can help providers alleviate much of the burden associated with EHR data entry and ensure accurate documentation of medical history, physical exams, medication lists, and more.


