Medical transcription services can help with transcribing any kind of clinical document, helping to streamline documentation and ensure better patient care. Among the many important documents are the discharge summaries. Professional EHR-integrated transcription services enable hospitals to create comprehensive discharge summaries – vital documents that are often overlooked by hospitals and, as a result, cause a negative impact on the patient’s post-discharge care.
Medical transcription services can help with transcribing any kind of clinical document, helping to streamline documentation and ensure better patient care. Among the many important documents are the discharge summaries. Professional EHR-integrated transcription services enable hospitals to create comprehensive discharge summaries – vital documents that are often overlooked by hospitals and, as a result, cause a negative impact on the patient’s post-discharge care.
Discharge Summaries are Absolutely Essential
Lack of a properly transcribed discharge summary can cause issues since in such cases patients are transferred without any clear instructions – the end outcome is affected and the risk of patient harm is also greater.
Discharge summaries provide clear guidance on how care must be rendered to the patient. Clinicians will have a clear idea of what treatment to administer, when to administer it, and what reaction to expect from the patient. It helps reduce anxiety and stress in workflow which would eventually affect the quality of care provided.
While patient portals and EHRs provide patients direct access to records, many of the physician notes are still concealed in discharge summaries. A complete discharge summary is also proof of the care and concern the hospital shows towards the patient and the steps it takes to ensure the patient has a great follow-up.
Incomplete Discharge Summaries Cause Fragmented Care
Fragmented care and treatment not efficiently coordinated has been one of the major causes of increased healthcare costs and patient harm according to the Health and Medicine Division (HMD). Apparently, even high performing health systems lag behind in the timeliness and transmission of discharge summaries as well as in the content quality. Sharing patient information is a vital aspect of care delivery. Inaccurate or delayed information transfer through the various care levels has a negative impact on re-admission, safety, efficiency as well as other quality dimensions.
Research conducted by the Yale University School of Medicine on heart failure exacerbation patients also states that quick distribution of detailed discharge summary to patients’ doctors improved outcomes of patients following a hospital stay and also reduced the chances of them being readmitted within a period of 30 days. In other words, the higher the quality of the discharge summary is, the lesser is the risk of complications which would necessitate readmission.
Essential Factors for Creating Discharge Summaries
Let’s look at the three essential aspects of the discharge summary – timeliness, smooth transmission, and content quality:
- Timeliness is a very important factor since hospitals must create a summary and provide a copy to the primary care provider of the patient to ensure better care quality. The Yale University School of Medicine research found that nearly 8% of the surveyed facilities did not have discharge summaries ready till 30 days had passed following the discharge.
- Transmission must be swift and smooth as well. Hospitals should ensure that they get the summary sent to the right practice or clinician for the next level of care after discharge. This does help in streamlining the recovery of patients while increasing their chances of receiving follow-up care.
- There can be no overemphasis on the content quality. Many discharge summaries are shockingly scarce on important details regarding the condition of the patient during discharge, any pending tests to carry out, further medication to be administered, or other follow-up recommendations.
Flawless Discharge Planning
In line with these factors, it would be wise to evaluate the discharge process of your hospital if there are issues in your discharge summaries. It is important to remember that the preparation for a smooth discharge starts right when the patient is admitted. The AHA (American Hospital Association) has brought out a few guidelines that hospitals must follow regarding discharge planning:
- To begin with, discharge planning must be based on the sound judgment of doctors, clinicians, nurses and other medical professionals of the care giving team.
- It is important to analyze the needs of each patient before you decide on their post-hospital placement following their discharge.
- Advanced resources such as EHRs need to be utilized to their full capacity for reducing or streamlining any administrative burden that could arise because of thorough discharge planning.
- Clinicians must collect all the required information, while the patient is at the hospital, regarding the choices that must be made for the post-discharge follow up care.
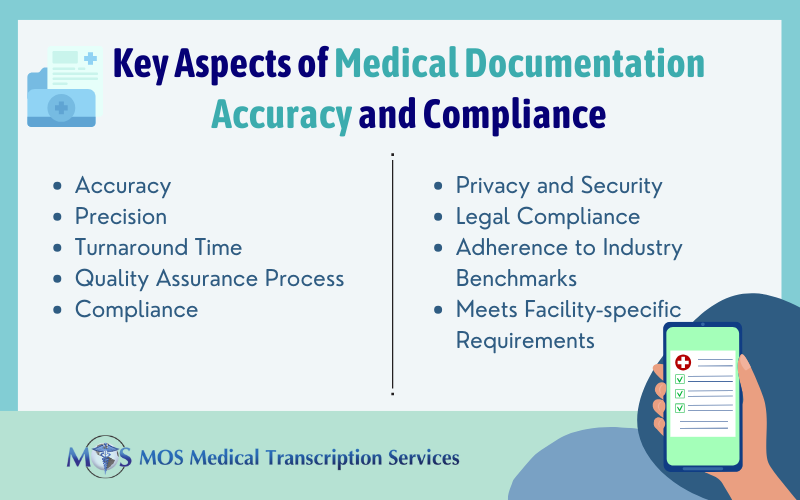
With these steps in place, discharge summaries can be transmitted more efficiently and smoothly. Professional medical transcription services can ensure prompt and accurate creation of these summaries, which will also help hospitals to be legally sound and have a strong record of the care they have provided.