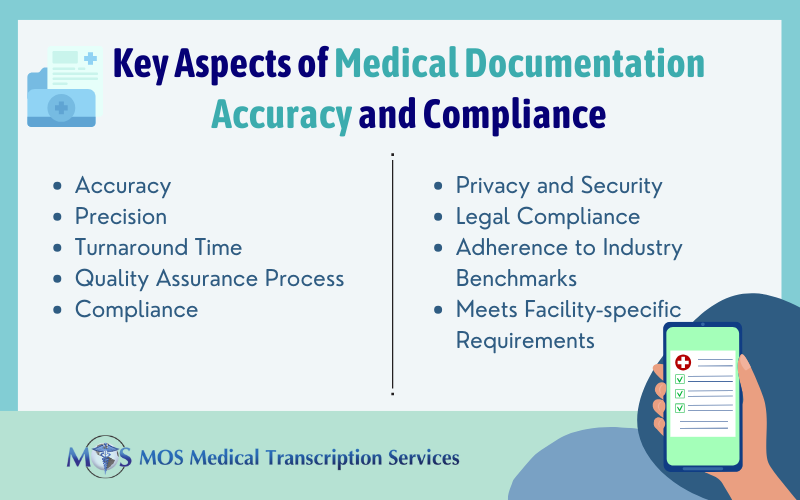
Quality is the most important concern in medical transcription. High error rates put patient safety at risk. Moreover, physicians would have to spend a lot of time and money to correct errors. In some cases, there are chances of transcription errors, while in others, they could be attributable to the author, that is, the healthcare provider. In a professional medical transcription company, the focus is always on improving physician documentation using better tools and techniques. The American Health Information Management Association (AHIMA), the Association for Healthcare Documentation Integrity (AHDI) and the Medical Transcription Industry Association (MTIA) have laid down the following guidelines to address medical transcription errors attributable to content errors.
Quality is the most important concern in medical transcription. High error rates put patient safety at risk. Moreover, physicians would have to spend a lot of time and money to correct errors. In some cases, there are chances of transcription errors, while in others, they could be attributable to the author, that is, the healthcare provider. In a professional medical transcription company, the focus is always on improving physician documentation using better tools and techniques. The American Health Information Management Association (AHIMA), the Association for Healthcare Documentation Integrity (AHDI) and the Medical Transcription Industry Association (MTIA) have laid down the following guidelines to address medical transcription errors attributable to content errors.
- Regular, practical feedback such as references cited and supplementary resources is provided whenever possible. Extracts of the transcribed version and the modified version with adequate surrounding context is included in the feedback. For proper understanding of corrected information, the sound file is also recommended. Special care is taken to see that the feedback is received and acknowledged.
- New medical transcriptionsts (MTs) who are unfamiliar with the job could be assigned mentors to help them to reach the expected levels.
- Sample reports should be distributed among difficult authors. Templates are provided if necessary.
- Policies and strategies for disciplinary action are developed to ensure that MTs meet quality expectations.
- Transcribers are assigned according to their knowledge in each specialty. A transcriber who has done chiropractic transcriptions may be able to handle physicial therapy transcription or orthopedic transcriptions. While asking them to do Neurological or cardiothoracic might have a longer learning curve.
Errors could be critical and non-critical. Errors which affect patient safety, care, or treatment can be put under critical errors and mostly involve the use of incorrect terminology, insertion of non-dictated information, omission of dictated information, or incorrect patient identification. Errors which affect the integrity of the documentation but do not alter the dictation meaning or affecting patient care or safety could be put under non-critical errors. Top medical transcription companies have multiple quality checks in place to ensure 99% accuracy in documentation.